Precision medicine represents a paradigm shift in healthcare delivery. In the simplest of terms, precision medicine tailors care for each patient based on knowledge of individual patient characteristics. It has the potential to completely transform healthcare delivery and health outcomes by treating the individual patient while reducing the burden on providers and the delivery ecosystem. It moves us closer to a prevention model and away from the aggregate approach to healthcare delivery that has characterized the last 50-plus years.
Precision medicine represents a paradigm shift in healthcare delivery. In the simplest of terms, precision medicine tailors care for each patient based on knowledge of individual patient characteristics. It has the potential to completely transform healthcare delivery and health outcomes by treating the individual patient while reducing the burden on providers and the delivery ecosystem. It moves us closer to a prevention model and away from the aggregate approach to healthcare delivery that has characterized the last 50-plus years.
According to the Precision Medicine Initiative, precision medicine is "an emerging approach for disease treatment and prevention that takes into account individual variability in genes, environment and lifestyle for each person." Precision medicine encompasses a broad group of connected health technologies: mobile health apps, electronic health records, electronic medical records, wearable devices, telehealth and telemedicine, and, of course, pharmacogenomics (PGx).
Despite the incredible efforts and investments that continue to be focused on the widening health disparities in the U.S., precision medicine doesn’t seem to find itself central to the conversation. It’s as if it’s massively misunderstood.
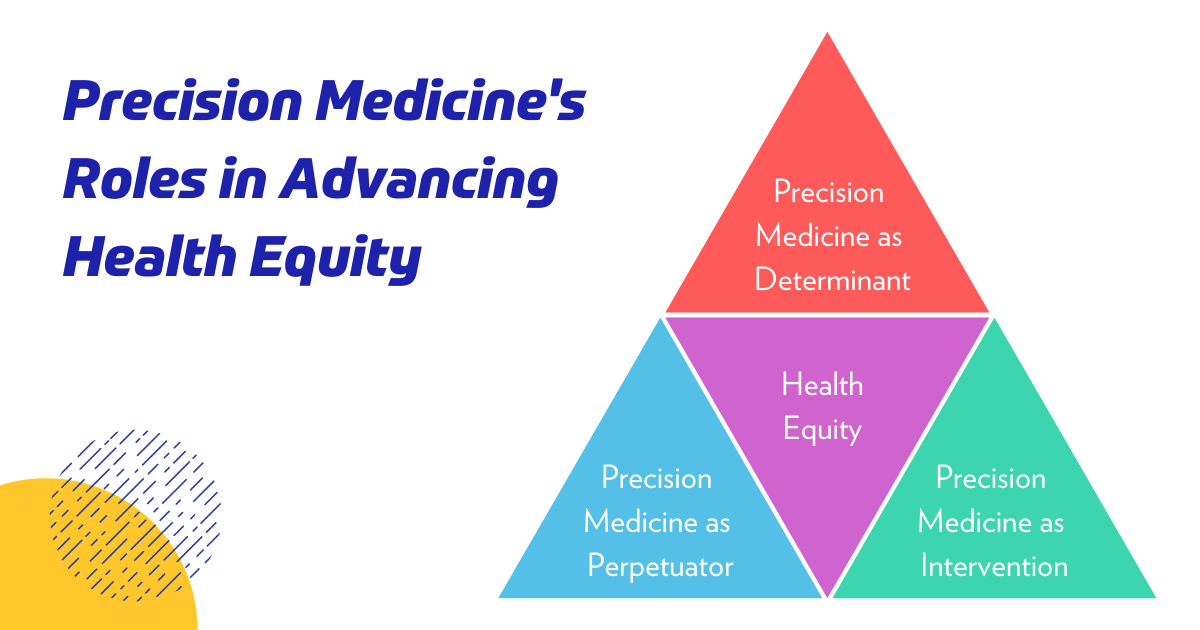
Understanding precision medicine’s place in the health ecosystem helps to uncover the three roles it plays in advancing health equity, which includes:
- Determinant
- Intervention
- Perpetuator
Determinant
According to a recent Brookings Institute Research Report aimed at understanding the connections between broadband and health equity, over 18 million homes in the U.S. are without a subscription for broadband. While this impacts all communities, more than 13 million “disconnected” homes are based in urban areas.
Accessing many precision medicine technologies requires access and health literacy. From telehealth to wearables to PGx testing, issues with access and digital literacy restrict participation. The lack of participation further exacerbates the divide, as data is not generated to support payment and adoption for these technologies in these subgroups. Beyond directly limiting access, low health literacy coupled with low digital access leaves patients quite literally “in the dark” on interventions that could greatly impact their health as well as the health of their communities. Patient demand and advocacy are huge drivers of health technology adoption in today’s consumer-focused marketplace. Patient demand drives physician demand, which is a key driver of payment. Without data and provider demand, there is little incentive for payers to cover these technologies.
HIMSS is currently engaged in a tremendous effort to ensure broadband access for all because it “affects nearly every social determinant of health, barriers to adoption and use represent significant challenges in individual and community-level outcomes.” In response to a Notice of Proposed Rulemaking on the Federal Communications Commission 5G Fund for Rural America, which would “use multi-round reverse actions to distribute up to $9 billion over the next decade and beyond to bring voice and 5G broadband services to rural areas of the country” in June 2020, HIMSS and PCHAlliance submitted comments in support of “the overall establishment and deployment of the [FCC 5G Fund for Rural America] fund.” HIMSS and PCHAlliance provided recommendations on the approach to deploying funds, encouraged FCC to lean on already established requirements, and stressed the importance of “tracking and evaluating cost savings to the healthcare system at large and the populations it serves through these programs.”
Intervention
Precision medicine technologies have the ability to incorporate many social, clinical and biological determinants of health to deliver a more customized care experience and to improve outcomes. Companies that develop these technologies are key partners, which invest in building connected health platforms and participate in value-based payment models.
Connected health products have the potential to impact short-term drivers of health disparities, keeping patients out of hospitals has wide-ranging impacts on health equity, caregivers, job security and so on.
As it relates to the HIMSS policy priorities of interoperability and connected health, an important pillar includes changes in reimbursement and Health Technology Assessment (HTA) policy to incentivize data integration and availability, particularly for medical technology developers and providers. Right now policy paradigms for reimbursement and HTA decisions at the federal and private level do not recognize the value, nor incentivize integrated data streams and new evidence models. In fact, many outright block the development of these important data streams and platforms that never allow such technologies and data to enter the market.
Medical technology companies are key partners in evolving infrastructure to enable connected health, but are not sufficiently addressing the barriers to adoption of these technologies, particularly at the policy level. Policies around reimbursement, including coding, coverage and payment, HTA, and rulemaking, such as the Stark Law and Anti-kickback statute, require huge investments that burn resources and drain companies. These resources could be put to better use, such as working in partnership with other stakeholders to develop the infrastructure to support connected health.
Perpetuator
The lack of representation of minority and underserved populations in scientific and clinical studies of precision medicine exacerbates health disparities. The primary way this occurs is through potential mistreatment, whereby clinical practice and guidelines are applied to individuals who were not represented in the underlying studies informing the current “best practice.”
In this era of big data and AI, if the pace of precision medicine development continues without addressing the underlying lack of representation in a meaningful way, we can expect health disparities to grow, not shrink. As these technologies and interventions are applied to these subgroups, albeit often in limited and inappropriate ways, the benefit of these technologies is unequally realized, widening the disparity gap. The obvious solution is to rebuild trust with these subgroups and find new, participatory, transparent, and culturally sensitive ways to engage them in research early and often.
After all, Henrietta Lacks, an African American tobacco farmer, who presented to Johns Hopkins with cervical cancer in the 1950s, and her immortal HeLa cells, taken without consent and later monetized, paved the way for precision medicine and simultaneously laid a foundation of mistrust amongst these subgroups.
Many efforts in this regard are underway, including the National Human Genome Research Institute’s work to engage with Alaska Native tribes, and Australian researchers’ efforts to increase participation in genetics research and trust in the Aboriginal Australian community. This is a long-term and necessary grassroots effort.
At the policy level, we must make health equity part of the value equation. Until gatekeeping organizations place overt value on health equity — e.g., through value frameworks and quality metrics — there will be little incentive nor opportunity to develop technologies to specifically advance health equity, particularly in light of current administrative complexity and costs to bring new technologies to market.
There are many digital technologies that can have measurable impact on health equity — e.g., to improve heart failure management in populations of African descent, a current unmet need — that may never see the light of day nor reach the populations who can benefit from them most because of how the current regulatory and HTA standards and processes work and how value is measured.
We all know the old adage: what gets measured is what gets done.
The views and opinions expressed in this content or by commenters are those of the author and do not necessarily reflect the official policy or position of HIMSS or its affiliates.
Global Health Equity Network
Help advance the cause of health and wellness for everyone, everywhere by advocating for underserved groups in health information and technology around the globe, and collaborate to find real-world solutions to challenges and roadblocks.