
Executive Summary
Since January 2011, Baptist Health South Florida’s (BHSF) system-wide Multidisciplinary Cardiac and Vascular Institute (MCVI) Best Practice committee has been working to improve all aspects of cardiac and vascular care including length of stay, 30-day readmission rates, cost-effectiveness and evidence-based practices. This committee is comprised of chest pain center coordinators, nurse practitioners, performance improvement experts, nurse informaticists, nursing directors and hospital administrators. In the fall of 2017, the organization’s evidence-based clinical care (EBCC) collaborated with the MCVI committee to work on physician order sets, known as PowerPlans™ to achieve their mutual goals. EBCC is a system-wide council that drives the implementation of evidence-based practice across the enterprise by incorporating them into the PowerPlans™. The purpose of this case study is to share the blueprint for successful improvement in the 30-day Centers for Medicare & Medicaid Services (CMS) heart failure readmission rate as experienced at the Homestead Hospital. The continuous improvement process has taken the 30-day CMS readmission rate from as high as 33.3% in 2011 to as low as 11.1% in 2019. The utilization of PowerPlans™ increased the bundle compliance rate from below the benchmark of 30% to rates as high as 60%.
Lessons learned include:
- Create a focus on patient education to include families and community awareness.
- Empower discharge RNs to conduct 1:1 patient follow-up-calls.
- Include 1:1 specific engagement from pharmacists.
- Screen for appropriate hospice and palliative care considerations.
- Implement standardized order sets (PowerPlans™) clinical decision support alerts, telehealth and population healthcare initiatives.
- Engage a full-time transition of care advanced practice registered nurse.
Define the Clinical Problem and Pre-Implementation Performance
The overall objective of the 30-day CMS heart failure readmission program was to create a sustainable process to successfully reduce the 30-day readmission rate in this population. Homestead Hospital’s multidisciplinary committee continuously developed and evaluated action plans to improve care and decrease the 30-day readmissions, which averaged 33.3% in 2011 and have been as low as 11.1% in 2019.
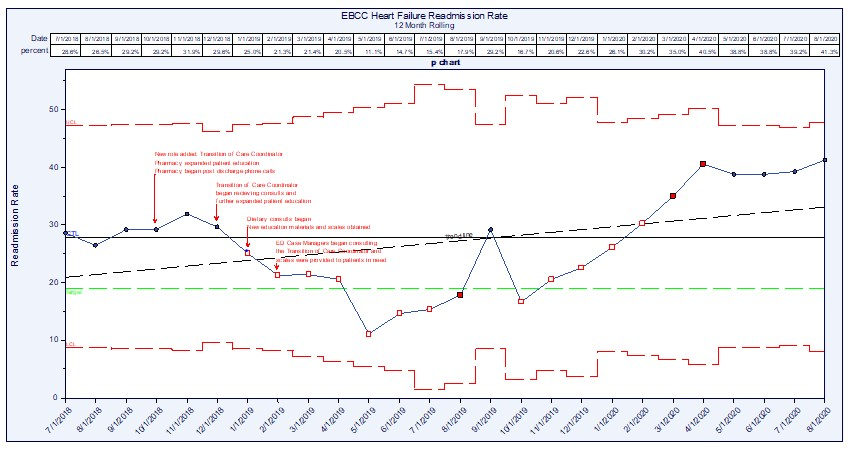
In 2016, the team re-focused on readmission prevention and implemented a Plan-Do-Study-Act Initiative and as a result several new processes were implemented over time (Figure 1).
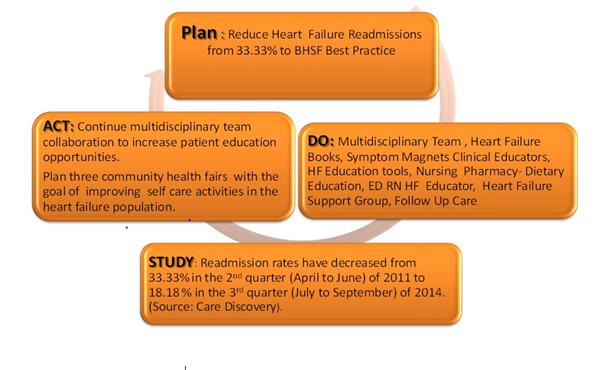
Source: Baptist Health South Florida
The initial work that focused on the 30-day CMS readmission rate was highly dependent on people and process and yielded good results in the overall reduction of the readmissions for the population. Analytics also played a role in providing the compass for sustainment and response to changes in the process. This is noted to be per care discovery data (Figure 2), which later transitioned into EBCC data. The EBCC data for 2016/2017 readmission rates ran in the 20% range.
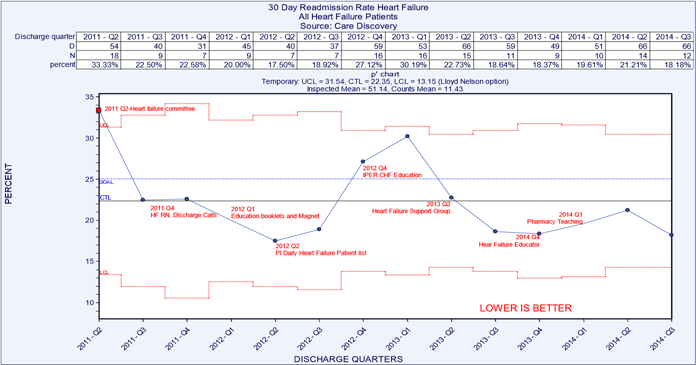 Source: Baptist Health South Florida
Source: Baptist Health South Florida
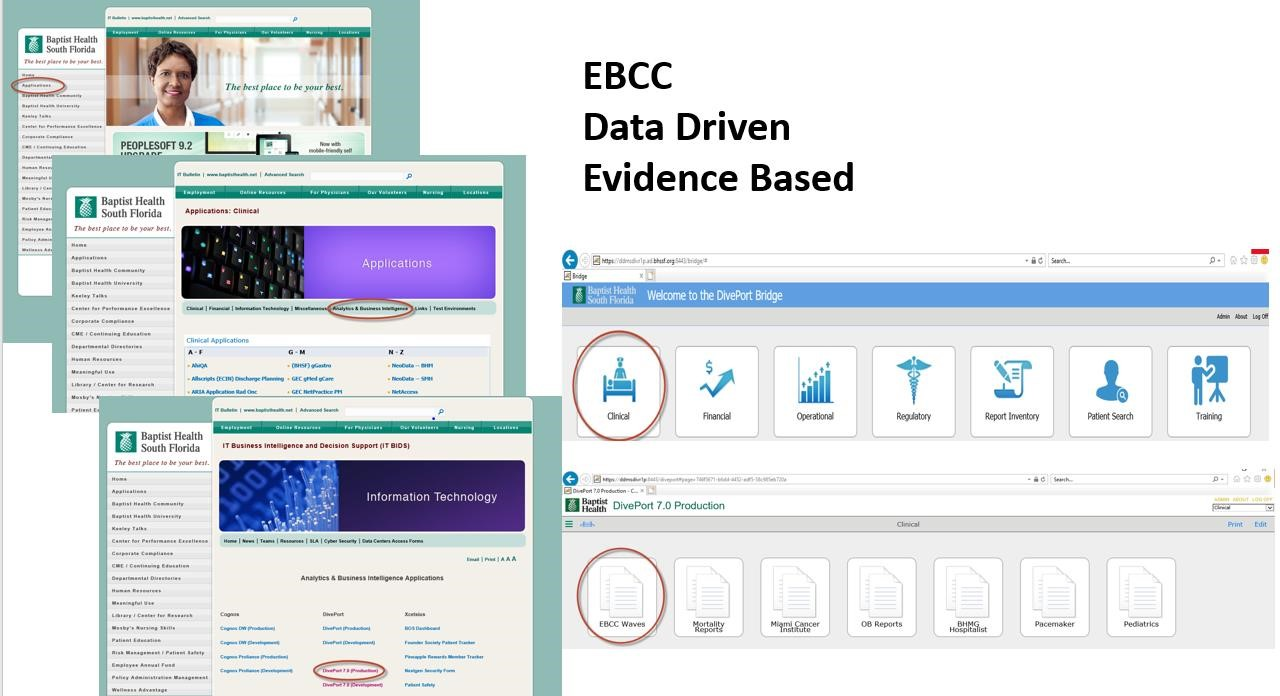
In 2016, BHSF implemented a new, fully integrated EHR on a scalable technology platform which further advanced the ability to move forward with improved management of the heart failure population. In the fall of 2017, the organization’s EBCC collaborated with the MCVI committee to work on physician order sets (PowerPlans™) to achieve their mutual goals. The utilization of the PowerPlans™ provided the tools to minimize the variation in care delivery. During this time the organization also moved to DivePort analytics, empowering the team with more robust data tools.
The DivePort database automatically calculates and generates the CMS 30-day readmission rate. The system uses the following formula in the calculation:
Numerator: Index accounts with a heart failure readmission X 100
Denominator: Index accounts **
** Index Admissions Included in the Measure
An index admission is the hospitalization to which the readmission outcome is attributed and includes admissions for patients:
- Enrolled in Medicare fee-for-service, Part A, for the 12 months prior to the date of admission and during the index admission
- Aged 65 or over
- Discharged alive from a non-federal short-term acute care hospital
- Not transferred to another acute care facility.
Index Admissions Excluded from the Measure
This measure excludes index admissions for patients:
- Admitted to prospective payment system-exempt cancer hospitals
- Without at least 30 days post-discharge enrollment in Medicare fee-for-service
- Discharged against medical advice;
- Admitted for primary psychiatric diagnoses
- Admitted for rehabilitation
- Admitted for medical treatment of cancer
The data steward is CMS. Evidenced-based guidelines follow the American Heart Association and the Institute of Healthcare Improvement. Benchmarking is also against the Premier database.
Prior to the implementation of the PowerPlans™ in August of 2018, the 30-day CMS heart failure readmission rate was measured at 26.5% and at peak performance with PowerPlan™ utilization the readmission rate was as low as 11.1% in May 2019. In late Q4 2019, there was a noted increase in the readmission rate to slightly above the current goal of 20%. This increase carried forward into early Q1 2020 as the COVID-19 pandemic began to impact healthcare organizations across the world.
Adherence to the compliance of care has improved from as low 18% in September 2018 to as high as 63% in November 2019 – with an organizational goal of 30% compliance. In 2018 Homestead Hospital expanded on nearly a decade of work in the management of 30-day CMS readmissions. Building upon the people and process initiatives already in place, the teams designed, implemented and began the analysis on standardized care delivery supported by a scalable technology platform.
Design and Implementation Model Practices and Governance
Background
Since January 2011, the organization’s system-wide MCVI best practice committee has been working on improving all aspects of cardiac and vascular care including length of stay, 30day readmission rates, cost-effectiveness and evidence-based practices. This committee is comprised of chest pain center coordinators, nurse practitioners, performance improvement experts, nurse informaticists, nursing directors and hospital administrators. In the fall of 2017, BHSF’s EBCC collaborated with the MCVI committee to work on physician order sets, later called PowerPlans™ to achieve their mutual goals. EBCC is a system-wide council that drives the implementation of evidence-based practice across the enterprise by incorporating the practices into the PowerPlans™.
Quality Improvement Activity
In January 2018, EBCC officially identified heart failure as one of the diagnoses to focus on for quality improvement. Consequently, EBCC completed development of the PowerPlans™ and each entity, including Homestead Hospital (HH), implemented the plans into the EHR. PowerPlans™ allow simultaneous ordering of all necessary components associated with effective clinical care of a particular disease or condition. They afford the prescriber efficiency with ordering the treatments. They also decrease variation in care, promote use of evidence-based practice and can lead to better outcomes. EBCC meets twice a month to determine diagnostic-related groups (DRGs) with the most opportunities for improvement, identifies best practices, establishes/reviews targets and plans the improvement strategies. The Critical Care Services Director represents HH at the system EBCC meetings. The Director serves as the liaison and facilitates the rollout of various EBCC initiatives in HH.
Interprofessional Team
HH’s Multidisciplinary Cardiovascular Collaboration Committee is an existing committee. It is comprised of hospital administrators, medical staff, nurses and representatives from the performance improvement, pharmacy, laboratory and dietary departments. This team meets monthly and/or ad hoc and utilizes the performance improvement model of Plan-Do-Check-Act to drive their initiatives. The committee has focused on the adoption of evidence-based practice in the management of certain cardiovascular conditions such as chest pain, myocardial infarction and heart failure in order to improve patient outcomes. For example, in August 2018 they supported EBCC in educating medical and nursing staff on the EBCC PowerPlans™. They reinforced the use of existing education materials for patients including standardized booklets, dietary and medication compliance and home reminders such as refrigerator magnets. In addition to the regularly scheduled meetings, some of the team members also participate in a monthly meeting with an outside performance improvement (PI) consultant engaged by HH to review metrics, drill down on the data and formulate tactics to expedite improvements.
Nurse Leadership
The designation as a Magnet facility represents the superb nursing leadership guiding the improvements in outcomes for Homestead Hospital. The Magnet Model is designed to provide a framework for nursing practice, research and measurement of outcomes. Through this framework, ANCC can assess applicants across a number of components and dimensions to gauge an organization’s nursing excellence. The foundation of this model is composed of various elements deemed essential to delivering superior patient care. These include the quality of nursing leadership, nursing coordination and collaboration across specialties. The 30-day CMS heart failure readmission prevention program was a key component in the Magnet Recognition process for Homestead Hospital. Nursing leadership guided much of the research and development, the education and the transformation of the existing process into a more robust effort. The addition of PowerPlans™ and approval for a pivotal role for a full-time transition of care coordinator APRN have proven to be key areas of benefit.
Education for the PowerPlans™ was completed via lunch and learns with classroom time, on-line formats on the EBCC website via the intranet and on the BHSF website which is available in the public domain. PowerPlan™ education is a consistent part of physician education and CME education is available with every MS-DRG or pathway as it rolls out. The PowerPlan™ go-live education began in August 2018 and the transition of care began driving the utilization of the PowerPlan™ in October 2018. Heart failure prevention education is also presented to staff in ‘what I need to know’ (WINK) material, and BHFS continues to support patients, families and the community in public educational opportunities.
The overall organizational structure for the EBCC is consistent throughout the organization and follows a consistent methodology for reducing variation in care delivery (Figures 3 & 4).
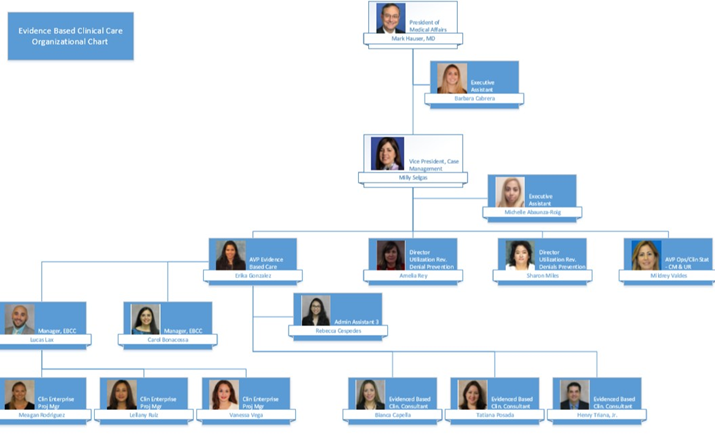 Source: Baptist Health South Florida
Source: Baptist Health South Florida
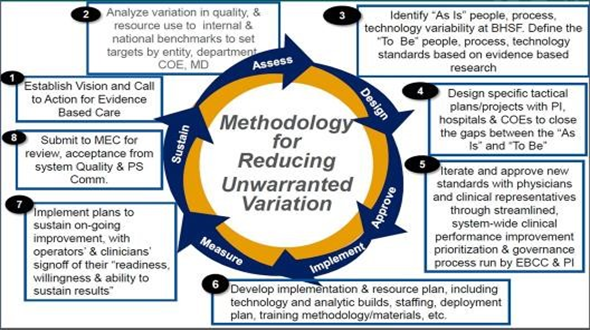
Source: Baptist Health South Florida
Clinical Transformation enabled through Information and Technology
Homestead Hospital (HH) has spent nearly a decade working to better manage the heart failure patient population. The people, process and technology approach has evolved over time into a solid transformational process geared toward high performance outcomes. In 2011 as HH faced a 30-day readmission rate of 33.3%, the MCVI Best Practice Committee began to instill educational based processes to lower the readmission rate.
From 2011 to 2014, the following heart failure initiatives were implemented:
- Core measure nurse
- Daily notification of all patients’ locations by PI department
- Patient education book
- Symptom magnets for home use
- Discharge call back nurse
- Support group
- Pharmacist medication education
- Dietary education by dietitian
- RN teaching script
- Follow up care referrals – home health, PCP and when appropriate palliative care
- Interdisciplinary Patient Education Records (IPER) chart audits
- A dedicated nurse patient educator
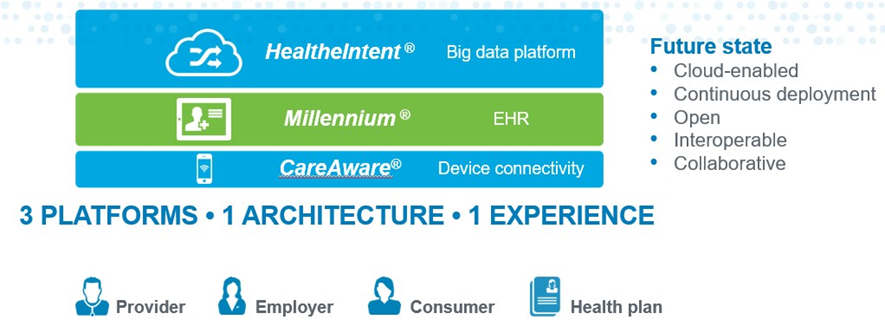
The people and process changes led to an improvement in the 30-day readmission rate to 18.18% in late 2014. In 2016, the implementation of the new EHR on a scalable platform created a foundation for continued growth and outcome improvements. The addition of device integration and population health platforms brought BHSF full circle in the capabilities to offer advanced technologies such as clinical decision support alerts, predictive algorithms, automated order sets, care plans, real-time device integration and population health tools such as registries and telehealth (Figure 5).
 Source: Baptist Health South Florida
Source: Baptist Health South Florida
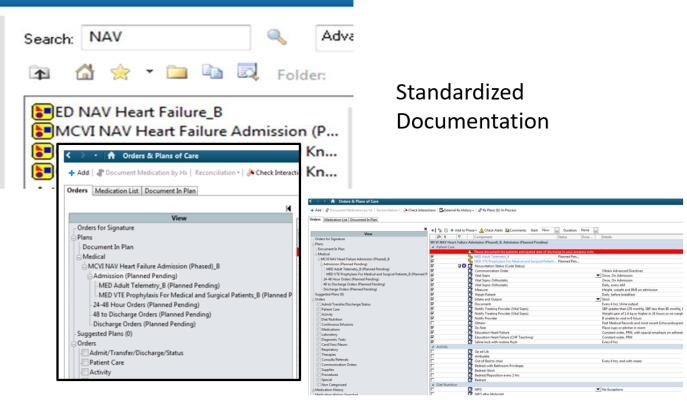
The PowerPlans™ support standardized evidence-based practice for treatment of a diagnosis, condition or problem. For example, the PowerPlan™ can be initiated upon arrival to the emergency department (Figure 6).
 Source: Baptist Health South Florida
Source: Baptist Health South Florida
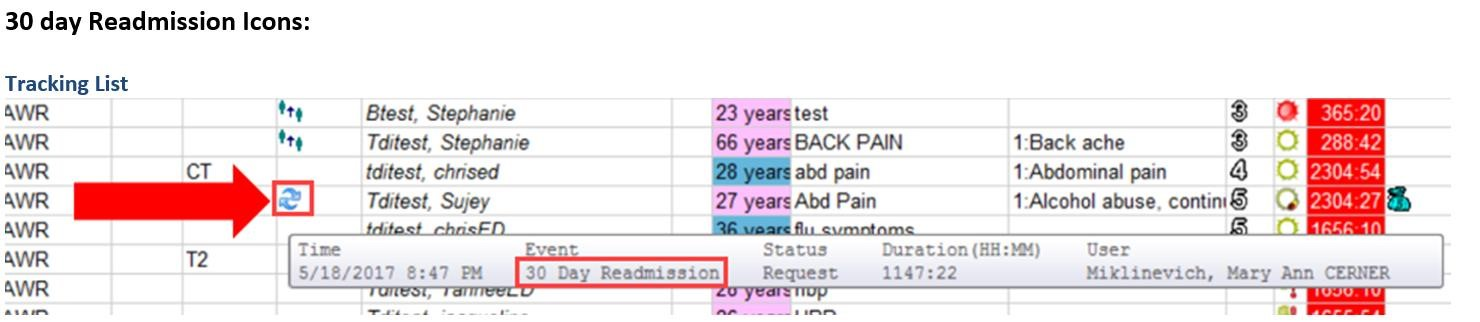
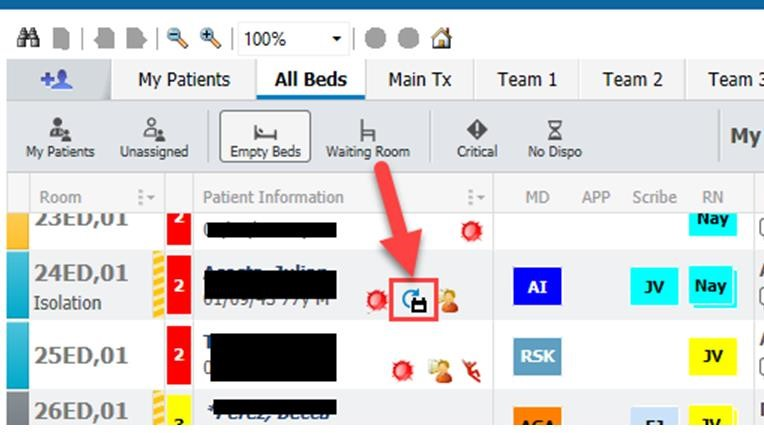
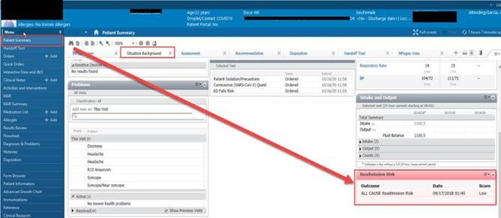
Patients with readmissions are also flagged in real-time on dashboards and within the workflow to case management and care providers (Figures 7 & 8).
 Source: Baptist Health South Florida
Source: Baptist Health South Florida
 Source: Baptist Health South Florida
Source: Baptist Health South Florida
The teams also have access to predictive information such as the risk of readmission and the data elements pulled from the integrated platforms (EHR, devices and population health/payor data) (Figures 9 & 10).
Source: Baptist Health South Florida
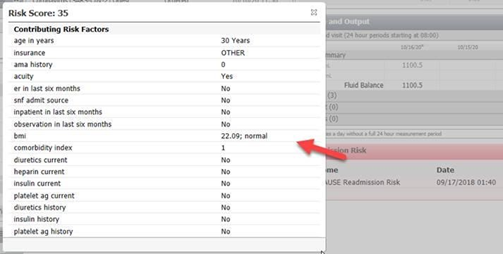
Source: Baptist Health South Florida
The All-Cause Readmission Risk Predictor algorithm pulls data from all three EHR data platforms (Figure 11):
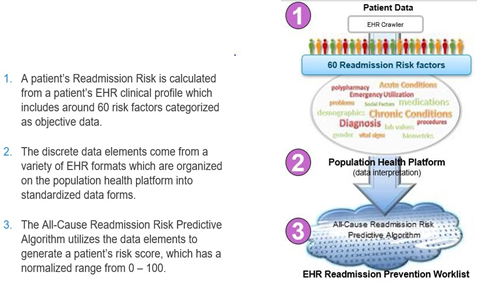
Source: Baptist Health South Florida
Prior to discharge, heart failure patients are aligned with the appropriate next level of care. Patients are assessed via the EHR’s transition patient worklist to enable a census screening that may be completed by the Baptist Home Care Coordinator. If the patient is heart failure or COPD, home health will also suggest Telehealth for the patient. Telehealth is a comprehensive remote patient monitoring program that is installed by our staff in the patient's home to collect, transmit and analyze vital signs and behavioral data. The program generates alerts when an intervention is needed and delivers meaningful information to the Telehealth nurse in the office via a secured Web portal. The Telehealth nurse can use this real-time data continuum to proactively connect the patient with the right intervention at the right time. The equipment is delivered to their home and they are typically monitored for 30 days to help prevent a readmission. The team will also follow up with the patient’s cardiologist/PCP as needed. Additionally, all Baptist Home Care patients are offered a Tele-pharmacy consult with our own Pharmacist who is stationed at the corporate office. The pharmacist provides a very in-depth discussion of all medications, side effects, omissions, duplications, drug-drug and food-drug interactions. These services are offered with no charge to the patient.
Improving Adherence to the Standard of Care
Measure of Effectiveness: The DivePort database automatically calculates and generates the PowerPlan™ compliance rate. The system uses the following formula in the calculation:
Numerator: Heart failure PowerPlan™ compliance
Denominator: Index accounts with a heart failure readmission
The PowerPlan™ was implemented in August of 2018 with a compliance rate of ~26% and an organizational goal of 30%. By May of 2019, the compliance rate was consistently greater than the organizational goal of 30% and HH has sustained compliance of greater than 30% with peak performance of 63% in November 2019. There is slight decrease down to 44% in January 2020 just as the COVID-19 pandemic began to impact healthcare organizations worldwide (Figure 12). BHSF benchmarks against CMS and Premier. Data abstraction methodology is based on claims data, registry data and chart abstraction.
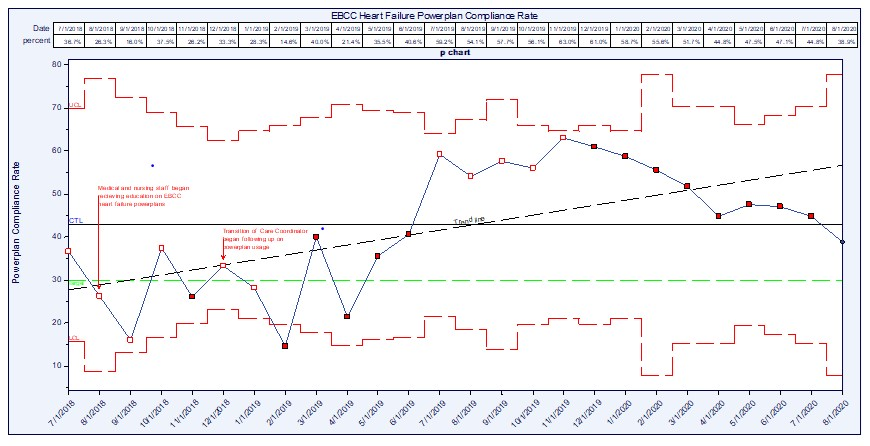 Source: Baptist Health South Florida
Source: Baptist Health South Florida
Improving Patient Outcomes
Measure of Effectiveness: The DivePort database automatically calculates and generates the CMS 30-day heart failure readmission rate. The system uses the following formula:
Numerator: Index accounts with a heart failure readmission X 100
Denominator: Index accounts
As the PowerPlan™ rolled out in the time period of August 2018 through November 2018, the 30-day readmission rate hovered above the organizational goal of 20% around the mid-30% range. With an increase in adherence to the utilization of the PowerPlan™, HH experienced a decrease in the 30-day readmission rate to below the goal of 20% to a low of 11.1% in May 2019. By November 2019 there appears to be a correlation between a decrease in PowerPlan™ compliance and an increase in 30-day heart failure readmissions. The time frame is also relative to the beginning of the COVID-19 pandemic that impacted healthcare organizations across the world (Figure 13). The achievement for the teams engaged in the process has been a journey of nearly a decade in the making. In 2011, the 30-day heart failure readmission rate lingered at 33.3%. Over time many advancements have been made to the processes, additional staff roles have been added and technology has now entered the age of digital transformation and patient engagement is nearly seamless. The domino impact of the COVID-19 pandemic is suspect in multiple data sets. The most recent work supports that increased compliance to the PowerPlan™ can result in a lower 30-day readmission rate. Access to the data, a heightened awareness to the outcomes and a focus on increased digital health should bring additional improvements.
 Source: Baptist Health South Florida
Source: Baptist Health South Florida
Accountability and Driving Resilient Care Redesign)
Care redesign for BHFS is driven by the EBCC initiatives. The EBCC is clinically driven and IT supported. Key stakeholders include:
- Facility Chief Executive Officers
- Chief Medical Officers
- Chief Quality Officer
- Centers of Excellence
- Finance
- Pharmacy
- Nursing
- Analytics/Business Intelligence Technology
- Chief Medical Informatics Officer
- Center for Performance Excellence
- Interdisciplinary physician members from each Baptist Health System facility
The purpose of the EBCC is to guide BHSF in a way that allows us to adopt to constantly changing science to improve the care we give our community. Our goal is to reduce variation in care, have better outcomes and realize efficiencies as a result. Patients get access to the highest standards of care, our physicians and care givers practice the state of the art and we take unnecessary costs out of the system. Our vision is that the EBCC will ensure that the organization’s healthcare providers deliver care that is deliberate and coordinated across all services, based on the latest clinical evidence, to provide superior clinical outcomes while reducing cost.
The adherence to evidence-based practice is crucial to our success. The EBCC takes pride in the responsibility of overseeing the implementation and success of our projects. Our responsibilities include:
- Establishing and following uniform evidence-based clinical standards of care, patient outcomes and experiences will be improved.
- Establish an interdisciplinary membership from each Baptist Health hospital medical staff and administration that will seek input and advice from leaders at each hospital in developing and implementing uniform system-wide evidence-based clinical standards.
- After considering the input received during the Review Period, the EBCC will present to the Quality and Patient Safety Committee for its review and approval, evidence-based clinical standards.
- Each hospital medical staff will track, encourage and over time enforce compliance with approved evidence-based clinical protocols through Ongoing Professional Practice Evaluation and Focused Professional Practice Evaluation.
The data to support the compliance to care is available in the DivePort analytics tool. DivePort provides data at multiple levels and is available to all key stakeholders upon completion of educational requirements (Figure 14).
 Source: Baptist Health South Florida
Source: Baptist Health South Florida
In August of 2020, BHSF announced the launch of its $100M digital transformation to become 'Amazon Prime of healthcare'. The focus of the future is truly on Digital Health Transformation. The blueprint created from initiatives such as the 30-day readmission prevention will lead the EBCC into the next phases of care delivery. The pandemic has opened the door to wider access to remote care delivery models. Patients with chronic conditions who may have postponed in-office follow ups, such as the heart failure patient, will be among those who benefit from a broader telehealth engagement.
The views and opinions expressed in this content or by commenters are those of the author and do not necessarily reflect the official policy or position of HIMSS or its affiliates.
HIMSS Davies Awards
The HIMSS Davies Award showcases the thoughtful application of health information and technology to substantially improve clinical care delivery, patient outcomes and population health.



