
Executive Summary
A multidisciplinary group of clinicians, administrators, care coordinators and informational technology experts worked together to address a complex healthcare issue that focused on patients who frequently utilize the hospital system. A small group of patients was identified, and upon initial review of their utilization data it was clear that St. Luke’s University Health Network (SLUHN) would benefit from a unified treatment plan to impact this repetitive cycle. Patients in this identified group were found to visit the emergency department as many as 24 times per calendar year and often had the same presenting complaints. These complaints resulted in duplicative testing and frequent readmissions. Additionally, the patients were found to have social and behavioral health barriers that impacted management of their healthcare needs.
To address the patient needs, an individual care plan is developed with a multidiscipline approach. Once finalized, the care plan is discussed with the patient and then made available to all clinicians, resulting in a unified, efficient approach in caring for the patient. The High Utilizer group learned that the electronic health record was an integral part of this program. The group worked on creative solutions to make the care plan easily accessible and succinct. Ultimately, the goals of the High Utilizer Care Plan (HUCP) group were achieved. The patients who had care plans demonstrated a decrease in ED visits, a decrease in inpatient admissions and a decrease in duplicative radiological testing. Most importantly, the patients received care that was unified, collaborative and safe.
Define the Clinical Problem and Pre-Implementation Performance
Among a small sampling of identified high utilizer patients, baseline data showed that these patients had between 20 and 29 hospital encounters within a 12-month period.
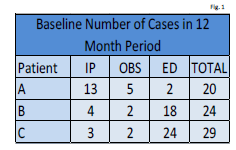
Source: St. Luke’s University Health Network
The HUCP group set a goal to demonstrate a reduction of ED visits, hospital observations and admissions by 25% improvement within a 6-month or 12-month period. While we started with a small group of three patients, the team has grown the program to include more than 150 patients through the course of the project.
One of the initial references that was reviewed and chosen as a guide was the definition by the Agency for Healthcare Research and Quality for ‘super-utilizers.’
- The identification of the patient cohort considered the number of Emergency Department Visits and/or Hospital Visits that a patient had over a period of 6 to 12 months.
- The team utilized a guideline of equal to or greater than three to six visits over the 6-month to 12-month period.
- All referrals were screened to determine inclusion versus exclusion in the program. The reasons for exclusion included:
- A patient with a substance abuse disorder, if the patient is not agreeable to rehabilitation treatment, was excluded. The reason for this is that a care plan would not be effective in decreasing or stopping the hospital utilization
- A patient who had medically necessary tests and visits during the 6-month to 12-month time period and was following up with providers in the outpatient setting was excluded
- A patient who was receiving hospice care during the screening process was excluded
Design and Implementation Model Practices and Governance
Clinicians and care managers identified patients for inclusion into the High Utilizer Care Plan program by utilizing EPIC, the electronic health record, Chart Review section, which clearly denotes admissions and ED visits for that patient. These visits are highlighted in red and obvious to the reviewer. The clinician and/or the care manager would identify the patient as a high utilizer when there were more than three visits to the ED resulting in subsequent admissions and many times duplicative testing for the same complaints within a 6-month time period. One example of a scenario that qualified someone for referral to the HUCP program was a patient who received as many as 24 CT scans of the head within a 12-month period for continued complaints of headaches.
Once these patients are identified, specific information is sent to the High Utilizer Care plan team. The information sent includes the patient’s name, medical record number and a brief description as to the referring person’s concerns regarding the patient. A secure email group was created for ease of sharing this information. The clinician and care manager, who are dedicated to writing care plans and outreach to the high utilizer patients, manage the database where all the care plans are kept. This same database has high utilizer patient referrals of those who have climbing utilization but with some specific intervention may not actually need a care plan. The care manager and clinician have a watch list for these patients and intervene accordingly.
The High Utilizer Care Plan team is a dynamic and cohesive group of 15 professionals from many backgrounds. The group is made up of care managers, parish nurses, administrators, emergency department physicians (including the Network Chair of Emergency Medicine), hospitalists (including the Network Chair of Medicine) and a clinical informatics nurse. This group is dedicated to confirmation of identification of the referred high utilizer patients, development of the care plan, communication to the care team and the patient. Data is tracked and reviewed comparing utilization and redundancy of high-end radiology studies from before and after care plan implementation. This committee utilizes what is referred to as interprofessional collaboration (IPC). IPC is essential because when a collaborative culture is created and communication strategies are put into place to support that culture, results can include:
- Improved patient care and outcomes
- Reduced medical errors
- Improved patient experience
- Reduced inefficiencies and healthcare costs
- Improved staff relationships and job satisfaction
Competency in IPC is the ability to function effectively within interprofessional teams, fostering open communication, mutual respect and shared decision-making to achieve quality patient care. Mutual respect and trust allow a team to identify and achieve mutual goals with a shared purpose.
The clinical informatics nurse was essential in developing the mechanism for viewing the care plan. The High Utilizer Care Plan group requested that the care plan be easily viewable within the EHR. The informatics nurse coordinated the discussion between the High Utilizer Care Plan team and the IT build team. A detailed proposal requesting an FYI flag, inclusive of a hyperlink to the care plan, was submitted. While the proposal was vetted, it was determined, due to technical reasons, that it was not possible for the EHR to have a hyperlink within the FYI flag. The workflow was adapted to include a hyperlink to the HUCP, which was housed within a best practice advisory (BPA). This was the “easy access” the clinicians requested. Prior to the High Utilizer Care Plan BPA build being released into the live EHR environment, the workflow was demonstrated by the build team to the High Utilizer Care Plan team. Once the BPA and the workflow were vetted and accepted by the HUCP team, education was provided to the clinical teams in the emergency departments, Hospitalists and Primary Care practices. Clinicians who join the network are given the High Utilizer Care Plan education upon starting to ensure there is continued adherence to the care plan and an understanding of the team’s goals.
Among a small sampling of identified high utilizer patients, baseline data showed that these patients had between 20 and 29 hospital encounters within a 12-month period. The HUCP group set a goal to demonstrate a reduction of ED visits, hospital observations and admissions by 25% improvement within a 6-month or 12-month period.
While we started with a small group of patients as indicated above, the team has grown the program from three patients to more than 150 patients through the course of the project. Clinicians identified high utilizer patients by examining emergency department and inpatient admission data of patients with multiple admissions; and of those patients, how many tests and what type of tests were performed. The High Utilizer team members responsible for delivering care to high utilization patients submitted formal requests for tools populating a High Utilizer Care Plan (HUCP) to the IT Governance committee.
The team used the technology within the Electronic Medical Record (EMR) to allow staff to identify patients as high utilizers and thereby having a Best Practice advisory and FYI flag fire on identification. This assists in alerting the care team of a patient with frequent utilization about a potential for uncoordinated care and readmission.
When the patient meets the following baseline criteria, the provider refers the patient’s case to the High Utilizer Care Plan Committee.
- Emergency department (ED) super-utilizers were defined as those patients with the highest number of ED visits in 2014, by payer: four or more visits for privately insured patients aged 1-64 years or Medicare patients aged 65 years and older; six or more visits for Medicaid or Medicare patients aged 1-64 years
- In 2014, although super-utilizers constituted a relatively small proportion of all patients seen in the ED (2.6 to 6.1 percent, depending on the payer-age group), they accounted for a large share of all ED visits (10.5 to 26.2 percent)
- Among Medicare patients aged 65 years and older, those with three or more chronic conditions constituted 33.3 percent of all ED visits among super-utilizers compared with 26.7 percent of ED visits among other patients
- ED super-utilizers accounted for 15 to 34 percent of all ED visits for abdominal pain and 13 to 29 percent of all ED visits for back pain
- ED super-utilizers aged 65 years and older accounted for 19 percent of all ED visits for urinary tract infections, 16 percent of ED visits for nonspecific chest pain, and 14 percent of ED visits for superficial injury
- Super-utilizers under age 65 years accounted for 19 to 40 percent of all ED visits for headaches
Following referral, the High Utilizer Care Plan Committee generates a standard care plan template for the initiating provider, the ambulatory care manager and the patient’s primary care provider. Input must be included from the patient's PCP and the Ambulatory Care Manager. The plan must be discussed with the patient before the next step can be completed. Prior to the new HUCP build being released into the live EHR environment, the workflow was demonstrated by the build team analyst to the High Utilizer team. The new tools were piloted on the first few patients to assess functionality of the tool.
Clinical Transformation enabled through Information and Technology
The EHR is instrumental in the identification, establishment and follow up of a High Utilizer Patient. The identification of these patients is multidisciplinary and anyone with access to the EHR can make a referral. Referrals are based on the Medicare/Medicaid definition of super-utilizers being defined as those patients with the highest number of ED visits in 2014, by payer: four or more visits for privately insured patients aged 1-64 years or Medicare patients aged 65 years and older; six or more visits for Medicaid or Medicare patients aged 1-64 years. However, clinical judgment can also be used as in the example of a patient with frequent imaging being performed or concerns for drug-seeking behavior.
Once the patient is identified, their case is referred to the High Utilizer Care Plan Committee for review. The referring person, clinician or care manager uses the HUCP group distribution to share specific information. This process starts with the designated medical provider, an Advanced Practice Clinician specializing in Hospital Medicine, reviewing the EHR. This review is comprehensive of the patient’s medical history, prior work up, baseline lab studies, imaging frequency and results, home medication lists and notation of outpatient providers. If appropriate, this medical provider will complete an individualized care plan for each of the identified patients. For less complicated cases, care manager intervention with coordination of outpatient follow up or connecting to Network or community services are arranged. This care plan is developed with input and review requested from the patient’s primary care provider (PCP) and any pertinent specialists concerning further management recommendations that should be followed.
Once a care plan is developed by the medical provider, it is brought to the High Utilizer Care Plan committee. If the team agrees with the developed care plan, the care plan is uploaded into the patient’s chart and a FYI flag titled “High Utilizer” is placed in the chart by the care manager. The medical provider calls the patient to discuss the care plan. During that discussion, the patient is made aware of the existence of the care plan and that all the providers in the St. Luke’s University Health Network can review it. Patients are also reassured that this is not meant to be punitive, but rather to make sure that they are always getting most appropriate and safe care.
When a High Utilizer patient returns to any of the St. Luke’s University Health Network facilities, upon opening the patient's chart, a provider will see the High Utilizer BPA (Best Practice Advisory). The provider should use the blue hyperlink to be taken directly to the High Utilizer Care Plan which will allow them to review the patient’s history, prior work up and treatment recommendations all in one place.
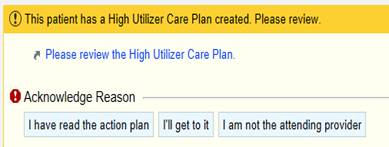
Source: St. Luke’s University Health Network
When the provider reviews the BPA, they can select "I'll get to it" if they do not have time to review, and this will delay the BPA for one hour. After one hour has passed, the BPA will appear when entering the chart again. This will delay the BPA to re-fire for 24 hours. If provider has already reviewed the note, then they select "I have read the action plan."
Providers and other members of the care team can also review the care plan in the notes section of chart review. The note can be found quickly by applying the “high utilizer” filter.
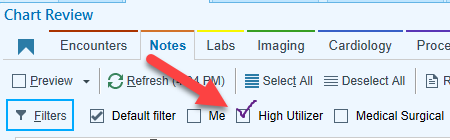
Source: St. Luke’s University Health Network
Reporting workbench reports are currently in place to assist clinical staff in managing this group of patients. The clinical staff can access these reports from their reporting library, edit the parameters to fit their needs and run the report to get immediate results. Within the workbench, the clinical staff can drill down using specific search criteria to identify patients who are higher risk within the HUCP empanelment and adjust care plan interventions as needed. Reporting Workbench reports can be duplicated adding ad hoc information requested by other departments. An example is adding Medicare Shared Saving Plan (MSSP) registry to show percentage of high utilizers that belong to other populations or alternative payment plans.
Registry and My Patient reporting are a functionality of the Healthy Planet application within Ambulatory Epic. Healthy Planet provides tools used in Epic that help clinicians manage populations and caseloads.
The “All Patients High Utilizer Registry” report tracks utilization, radiology and care management outreach activities that are then used to create Clarity reports that compare the metrics pre- and post-care plan implementation. Another Clarity report created based off of the registry aids in the monthly committee meeting prep. The report has decreased the time needed to prep for the meeting and improved the efficiency of care plan review. Clarity reports are reviewed quarterly by a subset group of the High Utilizer Care Plan committee to identify trends and opportunities.
The “High Utilizer FYI Flags” report is used by the Lead Ambulatory Care Manager as a clean-up report. Patients who become deceased are inactivated from the flag. Also, others can add the flag for other purposes. These are inactivated and allow the team to do education with others in the Network on the appropriate use of the flag and how to make a referral to the high utilizer care plan team.
The “My High Utilizer Patient” reports are utilized by the Care Management staff to organize and prioritize patient outreaches. An Episode type of “High Utilizer” in addition to adding the care manager to the care team serve to connect the patient to the report. The report also contains reason for next outreach and rows within the report turn yellow when the patient is due for outreach indicated in the care managers’ workflow by using track patient outreach. Regular outreach care managers assist in care coordination and reduce utilization by connecting patients with resources, providing disease management and helping alleviate social barriers to self-management.
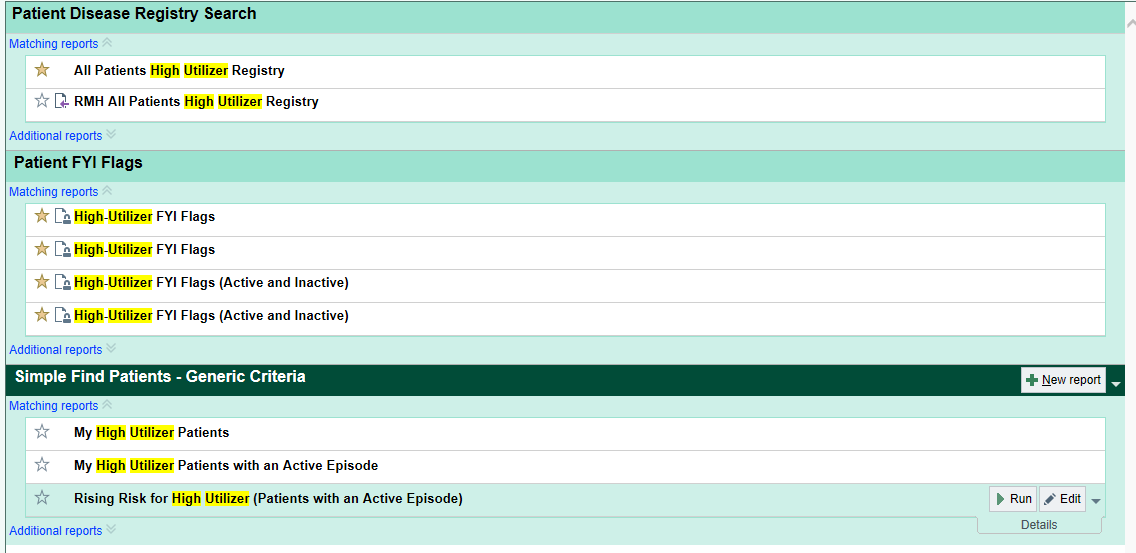
Source: St. Luke’s University Health Network
Chart abstracted data from the SLUHN EMR identified patients with limited resources, minimal healthcare follow up, and having multiple barriers related to social determinants of health (SDOH). Examples of SDOH include access to transportation and healthy foods or belonging to a marginalized group. After 90 days, the committee re-evaluates the patients (admits/readmits, ED visits, LOS and reduction in utilization of identified recourses) to decide if the patient still requires a care plan. SDOH are managed by the Network’s Care Management team by providing the following services for the high utilizer population:
- Safe discharge planning
- Safe transitioning across the continuum
- Community Resources
- Internal and external referrals for education or health coaching
- Disease management
- Medication Review
- Connecting to mental health resources
- Manage insecurities – financial, food, insurance, housing, medication, transportation
- Connecting the homeless with Parish Nursing
- Application assistance
- Home safety assessment including assessing for exacerbation triggers
- Assist with virtual visits in the home.
If it is determined the patient still requires care plan, then committee will re-activate the BPA for an additional 90 days.
Improving Adherence to the Standard of Care
The final care plan template was agreed upon by the multidisciplinary group. It went through several iterations, but the final version was one the group was most comfortable with. The group chose ease of use and succinctness as a foundation for the template given that the end user would be clinicians who are inundated with clinical information in the electronic health record. The HUCP group developed the process for dissemination of the care plan and the program. Campus-specific education sessions occurred once the care plan template, EHR optimization and process were finalized. During these education sessions, the clinicians were asked to adhere to the care plan as this was developed with the patient, with the patient’s care team and approved by the HUCP group.
The HUCP group measured adherence to the care plan by following the patient’s admission(s), ED visit(s) and radiological testing data. The data was obtained 6 months prior to the care plan development then compared to 6 months following care plan implementation. The improvement in all data areas implied the care plan treatment guidelines were being adhered to by those who were viewing the care plans. This combined with Tableau reporting enabled the HUCP to review the best practice alert activity that has the care plan embedded in it to see how often the clinicians are viewing the care plan vs bypassing the alert. It was found that in a time span of 5 months, the BPA fired 11,930 times. Thirteen percent of the time the clinicians used the provided link to view the care plan right away. The provider indicated that they had “already read it” 27% of the time. The providers chose “I am not the attending physician” button predominantly 40% of the time. Eighteen percent of the time, the clinicians stated they would get to it later. If the “I’ll get to it later” option is selected, the BPA will stop firing for that user for one hour before another reminder appeared. If they state they’ve already read it or are not the attending physician, the BPA will not fire again for that user for 24 hours. A required free text field is provided for the clinician to write in comments.
Chart 1: Provider types who chose to override the BPA from June 2020 to December 2020.
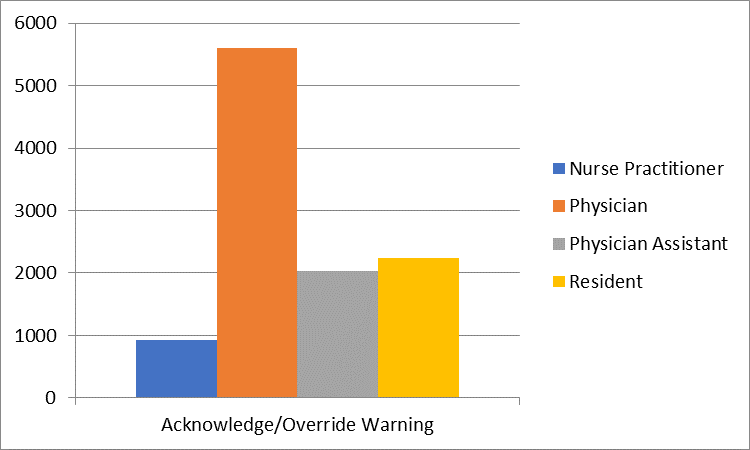
Source: St. Luke’s University Health Network
Chart 2: Provider responses to the BPA from June 2020 to December 2020.
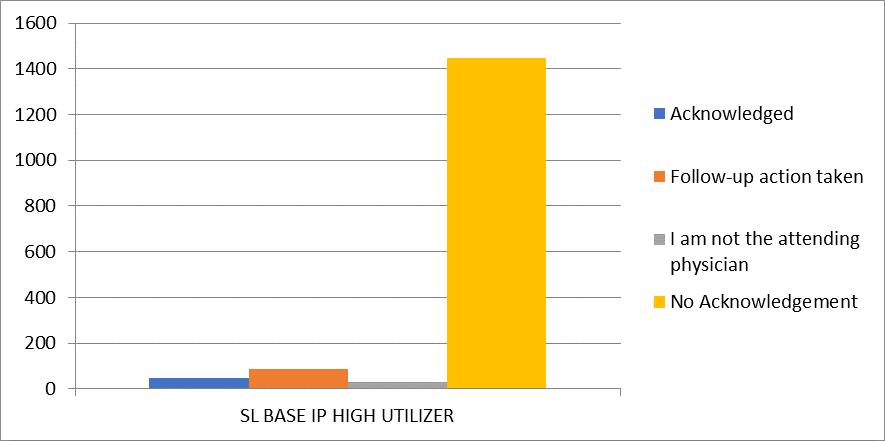
Source: St. Luke’s University Health Network
Chart 3: Number of providers who had no acknowledgement of the BPA between June 2020 and December 2020.
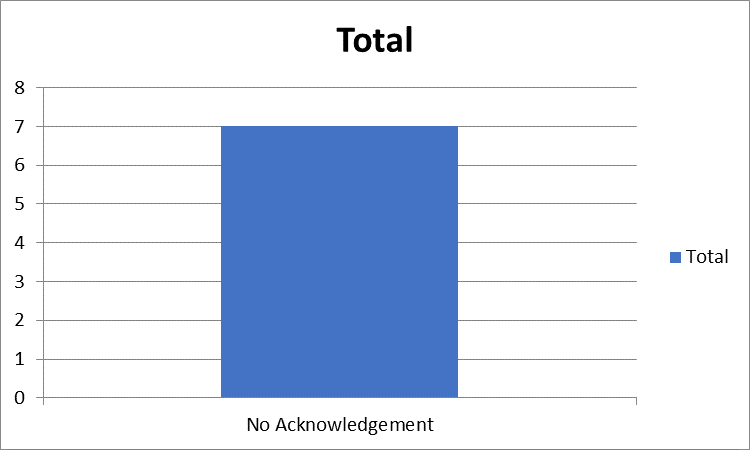
Source: St. Luke’s University Health Network
Tableau Reporting became available in the past 6 months to track provider adherence. The committee is working on a quality improvement plan to improve adherence. The committee will look at barriers in taking action on the BPA, reducing motion waste within Epic to improve ease of access to the care plan, showing a relationship between action on the BPA, reduction of utilization and redundancy of services.
As previously stated, the patient referrals for a high utilizer care plan come from care managers or clinicians. The HUCP group reviews the baseline information including clinical status and then determines if the patient would benefit from a care plan. Of the over 300 referrals, 151 have care plans developed. At the start of the program, it was determined that one clinician would be responsible for writing each individualized care plan and seek input from other members of the patient’s care team when appropriate. This was to ensure a single point of contact and for consistency with development of the treatment plan. Because each patient’s needs are different, the care plans are highly individualized based on that patient’s clinical status and social determinants of health. There is not one order set or pathway to follow in this regard. The consistent process is how the care plan is developed and then shared with the care team members. Additionally, the clinician who is dedicated to the HUCP development partners with a lead care manager who is focused on the social and behavioral aspects to the care plan. Having a consistent team develop the care plan and communicate back to the team has been one of the many successes to this program.
Improving Patient Outcomes
The High Utilizer patient cohort expanded from three patients to 88 with active user plans in May of 2019.
- For those 88 patients, of patients with a HUCP for 12 months, SLUHN observed 92% of patients reduced inpatient readmissions by a minimum of 25%
- 58% of patients reduced hospital observations by a minimum of 25%
- 75% of patients reduced ED visits by a minimum of 25%.
SLUHN observed similar impact for patients with shorter HUCP terms.
- For patients with a HUCP for 6 months, 79% of patients reduced inpatient readmissions by a minimum of 25%
- 36% reduced observations by a minimum of 25%
- 49% reduced ED visits by a minimum of 25%.
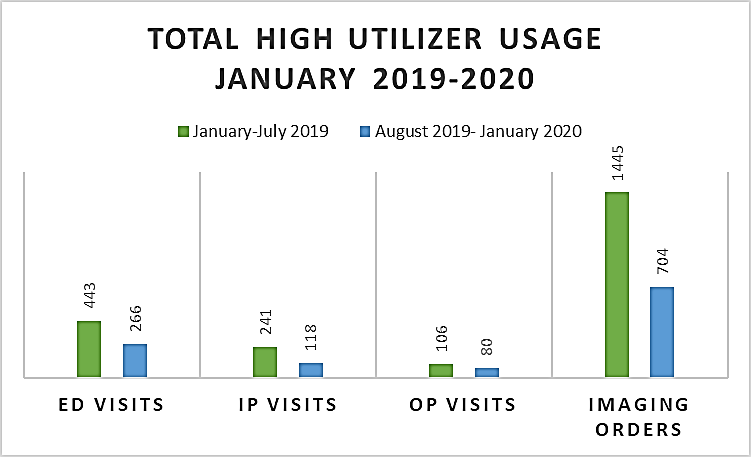
Source: St. Luke’s University Health Network
In July of 2020, the number of HUCP patients had grown to 151 patients. One of the many successes of the program has been the dedication of the medical provider and care coordinator. To be specific, the growth of the program increased due to adding these dedicated resources. The facilitator of the committee meetings along with the ambulatory care managers created a process to pre-review current care plans using a clarity report pulled from Epic. This process greatly increased the number of care plans that could be reviewed. An administrative assistant was also added to the team to capture the meeting discussion by way of meeting minutes. This allowed the committee time to review all the new care plans that are developed and discuss any amendments that need to be done. The minutes are then used to adjust the care plan suggested by members of the committee during the review before upload. To date, for patients who meet HUCP baseline criteria, hospital readmissions were reduced by 50%. High end radiology tests were reduced by 22%, and ED utilization was decreased by 25%.
Control Chart 1: Emergency Department Visits 9 months prior to care plan implementations compared to 9 months after care plan implementation using an upper, median and lower control level. “0” represents the start of the High Utilizer Care Plan.
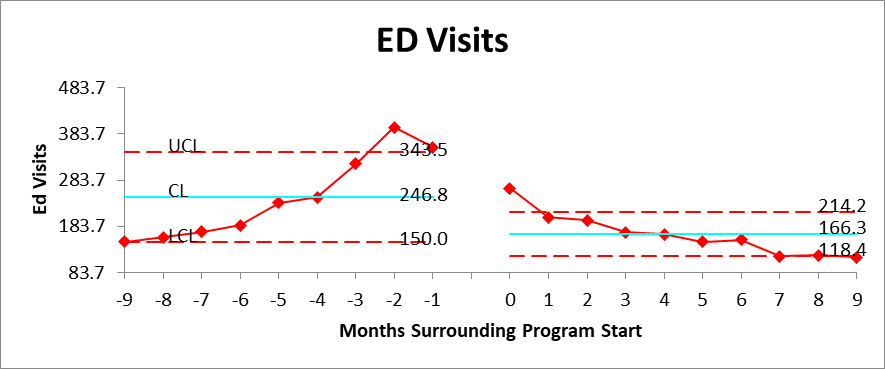
Source: St. Luke’s University Health Network
Control Chart 2: Admissions 9 months prior to care plan implementations compared to 9 months after care plan implementation using an upper, median and lower control level. “0” represents the start of the High Utilizer Care Plan.
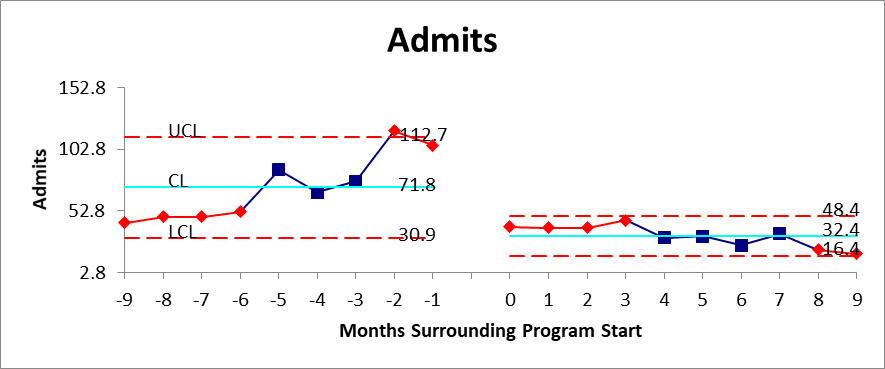
Source: St. Luke’s University Health Network
Control Chart 3: Readmissions 9 months prior to care plan implementations compared to 9 months after care plan implementation using an upper, median and lower control level. “0” represents the start of the High Utilizer Care Plan.
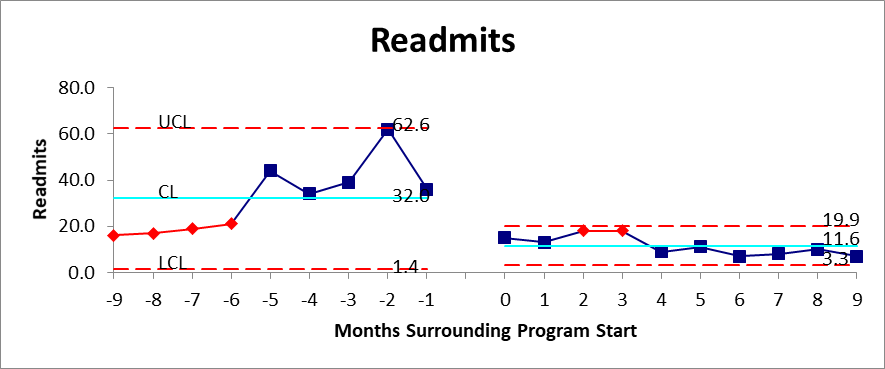
Source: St. Luke’s University Health Network
Accountability and Driving Resilient Care Redesign
Clarity reports have been developed to evaluate the care plan’s effectiveness comparing data of 6 months prior to care plan implementation to 6 months after care plan implementation. Also, the committee looks at the most recent 6 months of data on utilization and radiology studies for patients with at least 6 months of data post care plan. This data is used to look for trends that demonstrate utilization has increased especially on patients who have had a care plan beyond a year.
The data findings lead to a process improvement within the committee and the care management team. The dedicated medical provider will review the care plan and determine if changes need to be made. The provider will review the chart for accountability issues and connect with other providers on the care team for input on the care plan. If a care plan was not followed, the medical provider will discuss the treatment plan with the provider(s) who deterred from the plan and reinforce the need for adherence.
When an increase in utilization is identified, the care manager will provide outreach to the patient to discuss potential causes with the patient. Ambulatory care management workflow uses tools within Epic to receive alerts when a patient is admitted to the emergency department or hospital. This allows the care manager to collaborate with inpatient care management team on discharge planning or to outreach with the patient when the patient is discharged from the emergency department.
The data is shared throughout the network. Core members of the High Utilizer Care Plan committee act as a consultant to campuses who want to start their own high utilization oversight of patients who frequent those campuses. These subcommittees review patients biweekly and refer to the Network committee for a potential care plan. The subcommittees also identify barriers and resources both within the network and within the community that can help reduce utilization. Gaps in resources are identified and the subcommittee seeks others in the network who are subject matter experts in their discipline. Palliative care is an example of this and the palliative care team has started to work on a process similar for a subset of their patient population. The High Utilizer Care Plan committee and EPIC workflow can be a foundation for other services to build future projects.
In conclusion, the High Utilizer Care Plan Committee continues to develop tools, workflows and refine how patient data is captured to improve the process for patient identification, care plan development and goal achievement. Future state involves an increase of capture of SDOH within the electronic health record. This will allow the committee to measure the full impact of interventions and outcomes. The committee is dedicated to continual surveillance and evolution of the program by increasing provider adherence, improving patient engagement and experience and continued education of the network on the process.
The views and opinions expressed in this content or by commenters are those of the author and do not necessarily reflect the official policy or position of HIMSS or its affiliates.
HIMSS Davies Awards
The HIMSS Davies Award recognizes the thoughtful application of health information and technology to substantially improve clinical care delivery, patient outcomes and population health.



