
Executive Summary
While blood transfusion can be a life-saving procedure, liberal transfusion strategies are associated with increased length of stay, morbidity and mortality compared to restrictive transfusion practices. In the United States, blood transfusion has been named one of the top five overused medical procedures, and it is estimated that as much as 40% of all blood product transfusions may be unnecessary. These unnecessary blood transfusions cause direct patient harm, generate excessive costs for health systems and waste an important limited resource. Following the recommendations of the American Association of Blood Banks (AABB), The Joint Commission (TJC), the American Medical Association (AMA) and the National Surgical Quality Improvement Program (NSQIP), MU Health Care updated its standards of care and leveraged technology to help support its goals. On Dec. 19, 2017, Clinical Decision Support (CDS) alerts were implemented for RBC transfusion. The alert fires for patients with a hemoglobin level greater than 7.0 g/dL (or no hemoglobin level documented in the past 24 hours) when an RBC transfusion order is placed. CDS provides relevant evidence-based information to clinicians at the time of ordering to support best practice. Implementation of CDS has been associated with a decrease in the rate of unnecessary blood transfusions and improved patient outcomes. The goal was that by March 31, 2018, MUHC would reduce unnecessary red blood cell (RBC) transfusions by 10% through implementation of CDS for transfusion ordering and that teams would continue to provide additional blood product management tools overtime. In the initial work, MU Health Care decreased overall RBC transfusion by 20%, achieved a 10% reduction in mortality for transfused patients and reported cost savings of about$500,000. Specifically, in the orthopedic surgery population, MU Health Care realized the following successes:
- 4% reduction in patient average LOS
- 13% reduction in transfusions
- 10% reduction in patients with a transfusion with a pre-transfusion hgb> 8
- 3% reduction in the average hgb level prior to a transfusion
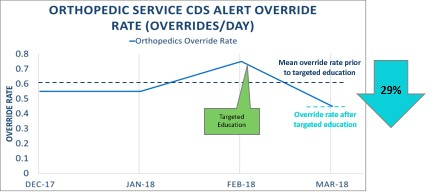
- 29% reduction in transfusions without a pre transfusion hgb
- 8% increase in single unit transfusions
Lessons learned include:
- Culture change was one of the greatest challenges — we made it fun while explaining the “why”
- Create a “campaign” to focus on the changes can bring additional visibility to your goals
- Teach the process to give one unit and then reassess
- Create a data driven process
- Reward those who excel at compliance
- Engage early with those who have opportunity to improve
- Don’t stop at Packed Red Blood Cells (PRBCs) — include CDS for Fresh Frozen Plasma (FFP) as well as platelets (PLTs )
- Anemia clinics are a great option for those patients who are anemic prior to surgery
Define the Clinical Problem and Pre-Implementation Performance
Armed with studies showing up to 40 % of transfusions in the U.S. are unnecessary, MU Health Care leaders saw an opportunity to improve patient safety and reduce costs by implementing a red blood cell (RBC) transfusion clinical decision support alert (CDS). Nine months after embedding the alert into the electronic health record, staff reduced the health system’s overall RBC transfusion rate by 13.34%, saving approximately $195,000 in acquisition costs and avoiding between $505,000 and $1.14 million in indirect costs for things such as transfusion administration, patient blood testing and overhead. In the original work, from December 2017 through February 2019, MU Health Care also noted a 10% reduction in the mortality rate of transfused patients. There were improvements in LOS, for example in the orthopedic surgery patient population. This reduction in LOS is attributed to a standardized care delivery process which includes the Patient Blood Management (PBM) standards as part of the routine order sets.
The alert, designed to reflect evidence-based guidelines, appears when clinicians place RBC transfusion orders for admitted patients with a hemoglobin level greater than 7.0 g/dL or no hemoglobin level documented in the past 24 hours — excluding orders for patients in the neonatal intensive care unit, operating room and emergency department. The guidelines and standards are as reflected in the PBM Certification offered jointly with the American Association of Blood Banks(AABB) and The Joint Commission (TJC ). Four other highly respected societies in healthcare have also committed support in decreasing unnecessary transfusions: 1) The Society of Critical Care Medicine 2) American Society of Anesthesiologists 3) American Society of Hospital Medicine and 4) American Society of Hematology. Orthopedic care has also been recognized by US News and World Report as well as by the DNV-GL.
The goal defined to assess adherence to the quality standard and decrease blood utilization is MU Health Care’s transfusion rate by month. The rate is based on the total number of RBCs transfused (the numerator) and the total number of inpatient discharges (the denominator). Exclusions are orders for patients in the neonatal intensive care unit, operating room and emergency department. The targeted improved performance is a decrease in length of stay, a decrease in mortality and cost avoidance in unnecessary spend.
Design and Implementation Model Practices and Governance
Since The Office for Clinical Effectiveness (OCE) oversees many of the quality improvement and patient safety initiatives. The OCE worked with leadership in the blood bank and the transfusion committee to stand up the PBM process. The EHR supplier also had an interest in this space and partnered with MU Health Care to assist in the technology requirements and the build and design of the analytic tools for process improvement. MU Health Care created a role for the Transfusion Safety Officer (TSO) in February of 2017 and initiated the preop anemia consult service in June of 2017. The CDS alert for RBCs was implemented in December of 2017.
The members of the Transfusion Committee who currently oversee the process, is made up of:
- The Chairperson – Associate Professor of Clinical Surgery
- Assistant Professor of Clinical Pathology
- Clinical Pharmacy Specialist
- Interim Division Director & Professor of Clinical Medicine
- Medical Technologist – Blood Bank
- Professor of Clinical Medicine
- Supervisor – Laboratory – Blood Bank
- Associate Professor of Clinical Child Health
- Professor of Clinical Pathology & Anatomical Sciences
- Manager, Laboratory Services
- Director of Nursing
- Informatics
- Senior Performance Improvement Leader
Additional participating committees include clinical decision support and alert fatigue prevention, informatics for build and design and analytics to ensure that the processes and follow-up are data driven.
The education rollout was conducted by the TSO and the Medical Director of Transfusion services. The educational sessions took place as presentations in grand rounds, at huddle time and visual cues within the facilities. Much effort was also focused on culture change. The routine order for RBCs in the past had been “2 units of packed red blood cells (PRBCs ) – making the culture shift was the most challenging from the people, process and technology aspects. Visual cues included posters and badge buddies for reminders with cues such as “Think outside the bag,” “Roses are red, violets are blue, don’t use two units when one will do.” Data was utilized to identify those who were doing well with the new PBM guidelines, and they were rewarded with goodie bags and a positive shout out. For those with areas of opportunity, group and one-on-one discussions were held as needed. The education campaign took about three months.
Clinical Transformation Enabled Through Information and Technology
On Dec. 19, 2017, the CDS alert was implemented for RBC transfusion. The alert fires for patients with a hemoglobin level greater than 7.0 g/dL (or no hemoglobin level documented in the past 24 hours) when a RBC transfusion order is placed. NICU patients are excluded from the alert, as are all operating room and emergency transfusion orders. Clinicians who encounter the alert can either cancel their order with a single click or proceed by selecting an override reason. The alert helps reduce RBC transfusions in two ways: It provides clinicians with best-practice guidance as they’re placing the order, influencing their immediate behaviors while simultaneously informing or deterring future orders. The process also generates data showing how clinicians interact with the alert, highlighting opportunities for additional education.
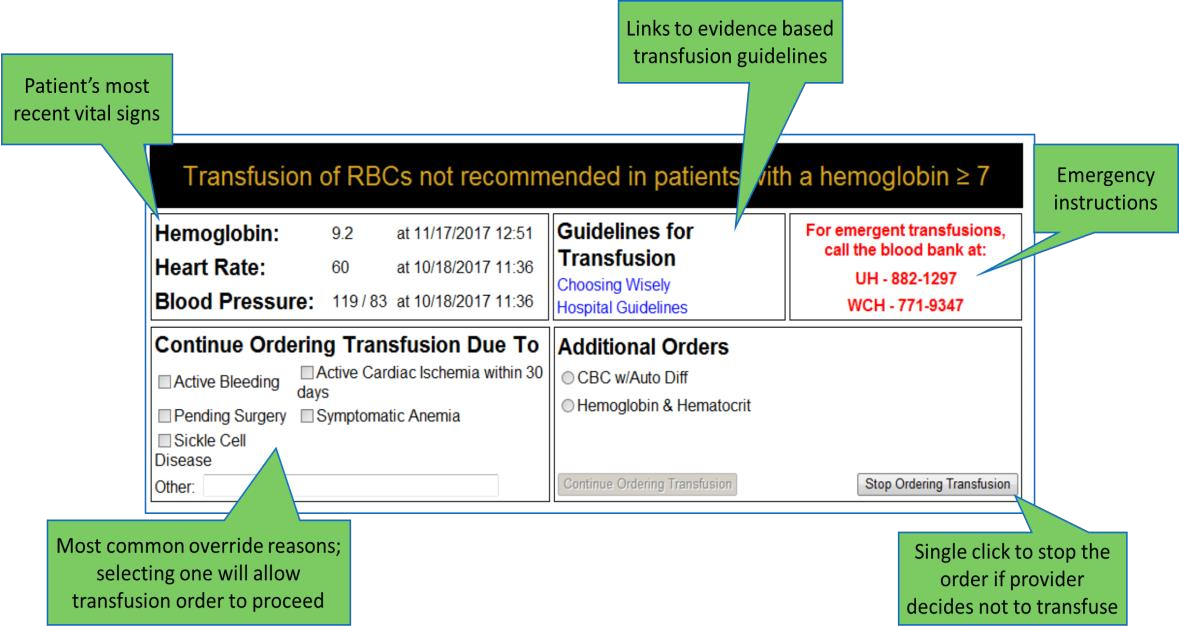
Source: University of Missouri Health Care
In addition to the CDS alert for RBCs that went live in December 2017, the FFP alert was released November 2018, and the alert for PLTs was released October 2020.
The workflow for the pre-op anemia consult ensures those patients with anemia are properly treated prior to their arrival for surgery, providing another option to decrease blood utilization.
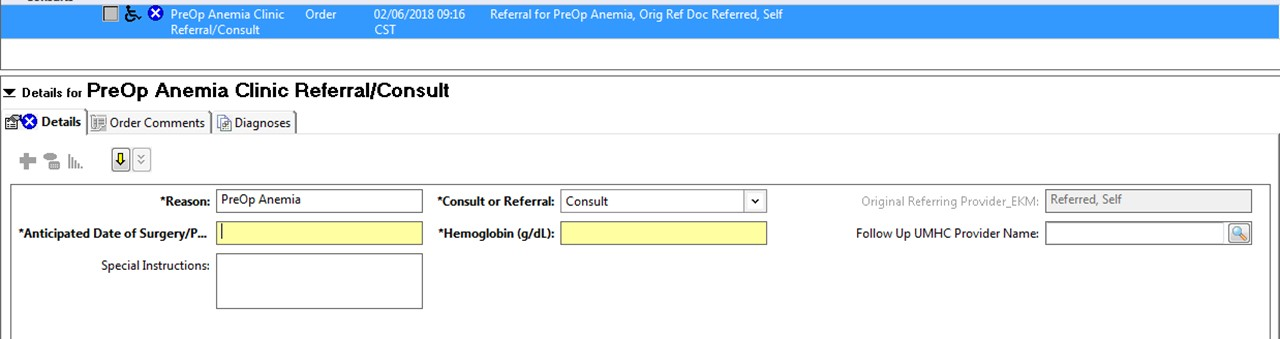
Source: University of Missouri Health Care
Pre-op Anemia consult workflow:
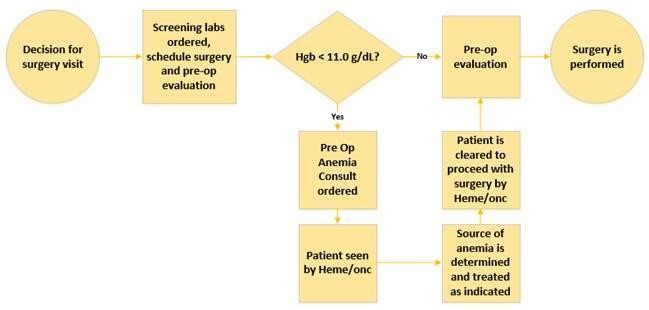
Source: University of Missouri Health Care
Technology is also in place to ensure the right blood products are given to the right patient. Through bar code scanning and positive patient identification, MU Health Care has been compliant with scanning rates for blood administration (current HIMSS Stage 7 EMRAM).
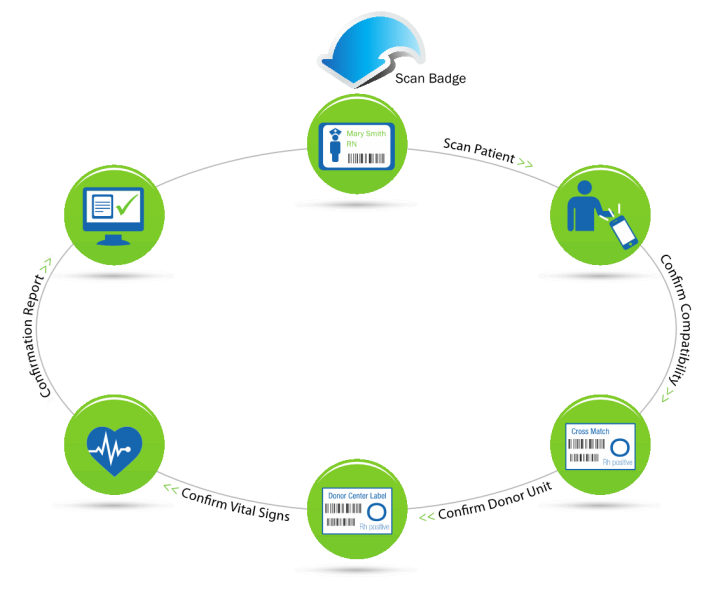
Source: University of Missouri Health Care
Improving Adherence to the Standard of Care
The primary goal defined to assess adherence to the quality standard and decrease overall blood utilization is MU Health Care’s transfusion rate by month. The rate is based on the total number of RBCs transfused (the numerator) and the total number of inpatient discharges (the denominator). Exclusions are orders for patients in the neonatal intensive care unit, operating room and emergency department. The standard of care is based on recommendations from the AABB and other key healthcare societies. The data is obtained via electronic chart abstraction (EDW), claims data and population health data. MU Health Care participates in Vizient for benchmark data.
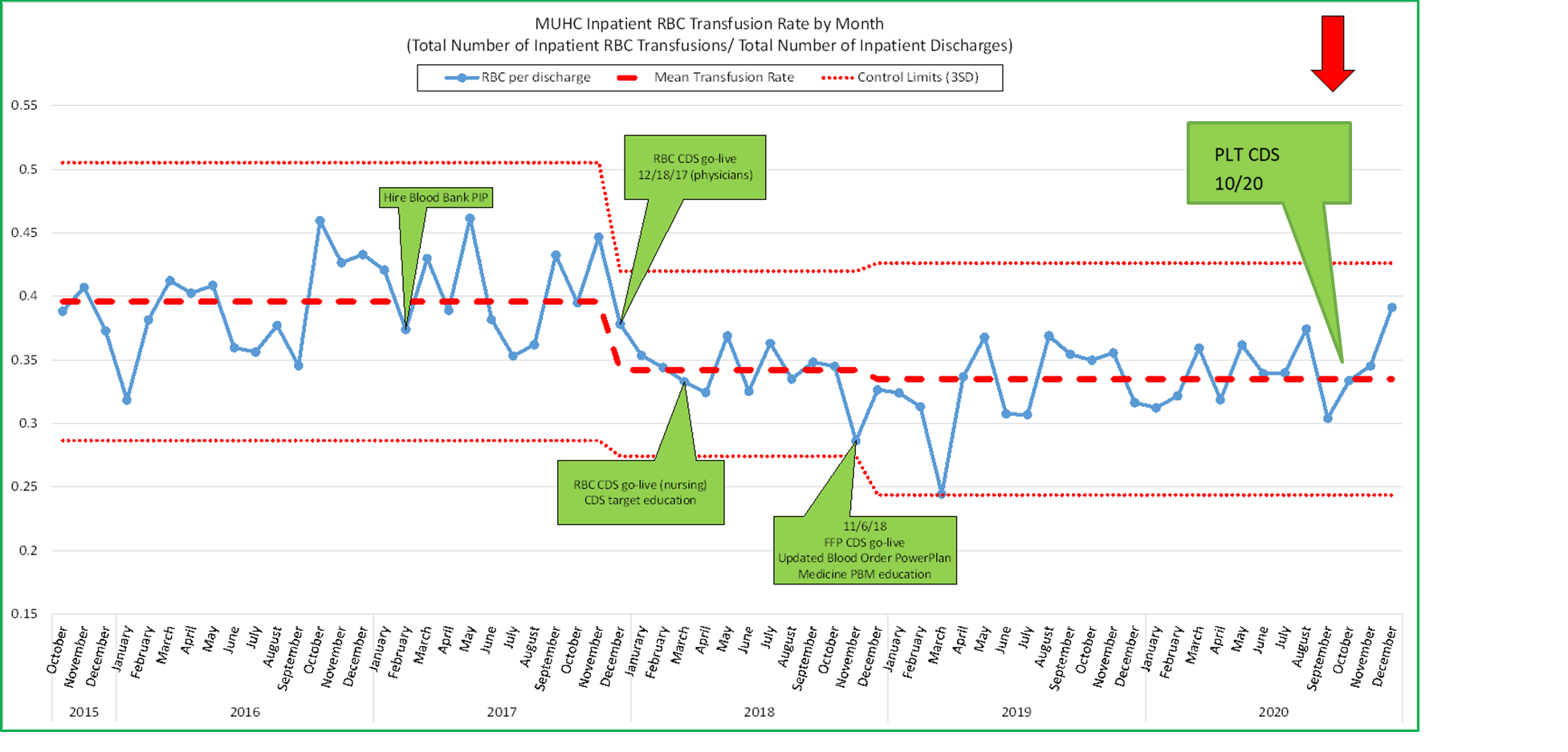
Source: University of Missouri Health Care
Additional indicators of positive adherence are noted in the orthopedic surgery patient population include:
- 10% reduction in patients with a transfusion with a pre-transfusion hgb> 8
- 3% reduction in the average hgb level prior to a transfusion
- 29% reduction in transfusions without a pre transfusion hgb
- 8% increase in single unit transfusions
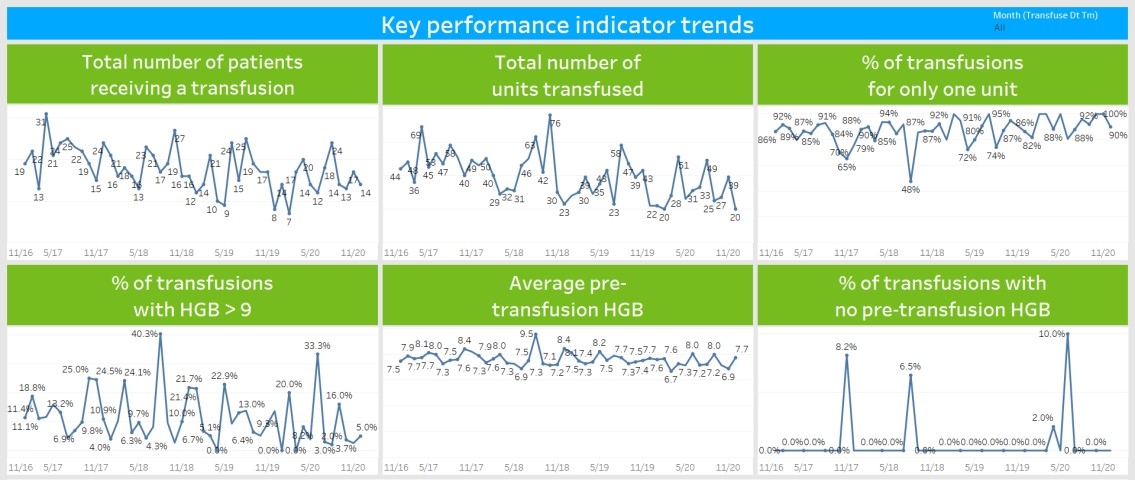
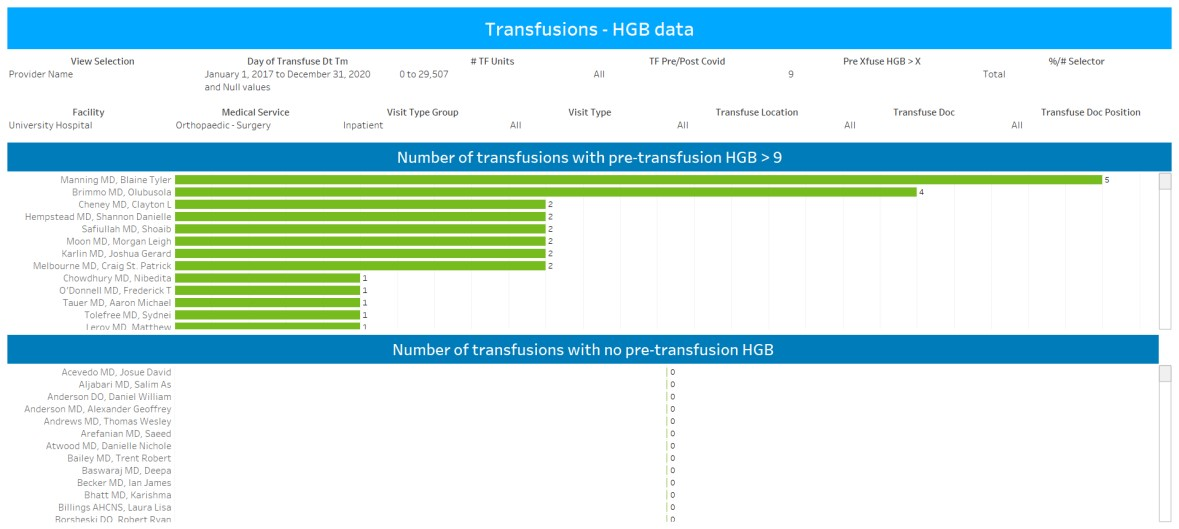
PBM process is data driven (Blood Management Utilization Dashboard):

Source: University of Missouri Health Care
Improving Patient Outcomes
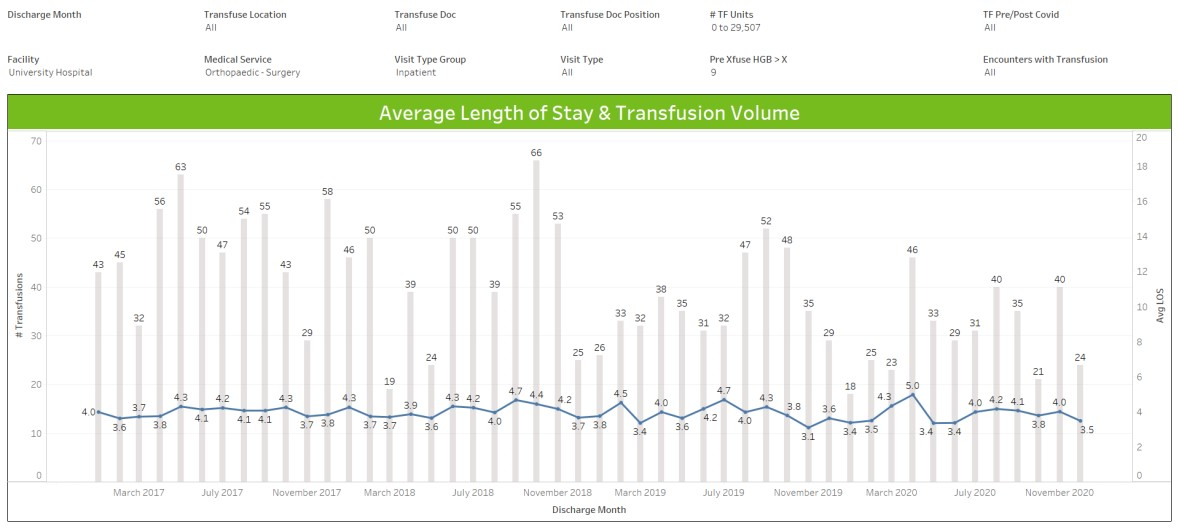
MU Health care defined the improved outcomes as a decrease in length of stay for patients who did not receive a blood transfusion, decreased mortality and cost savings. The orthopedic surgery patient population is presented as a subset due to high volume and previously high utilization of blood products. This was also a group who received additional education to the standard.
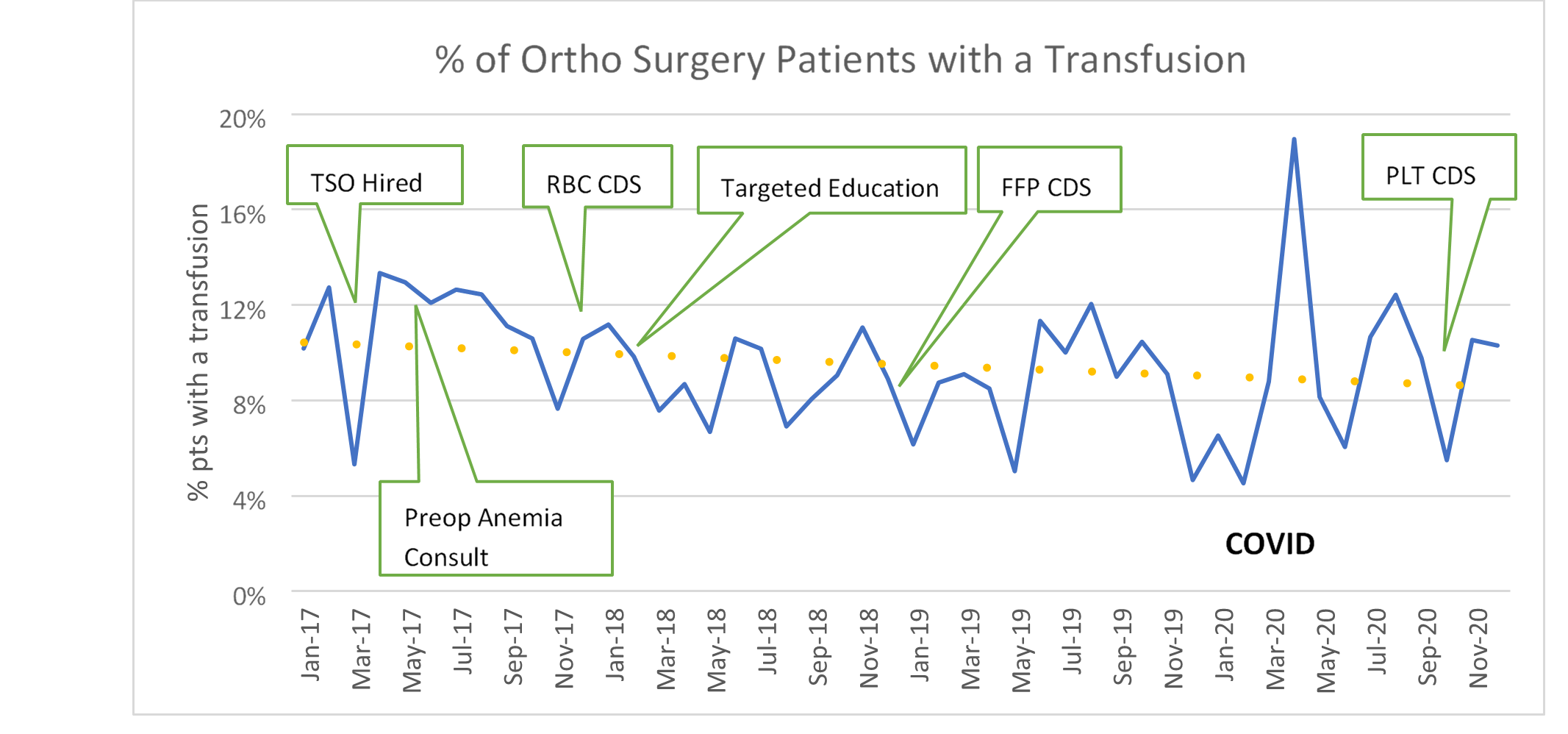
Source: University of Missouri Health Care
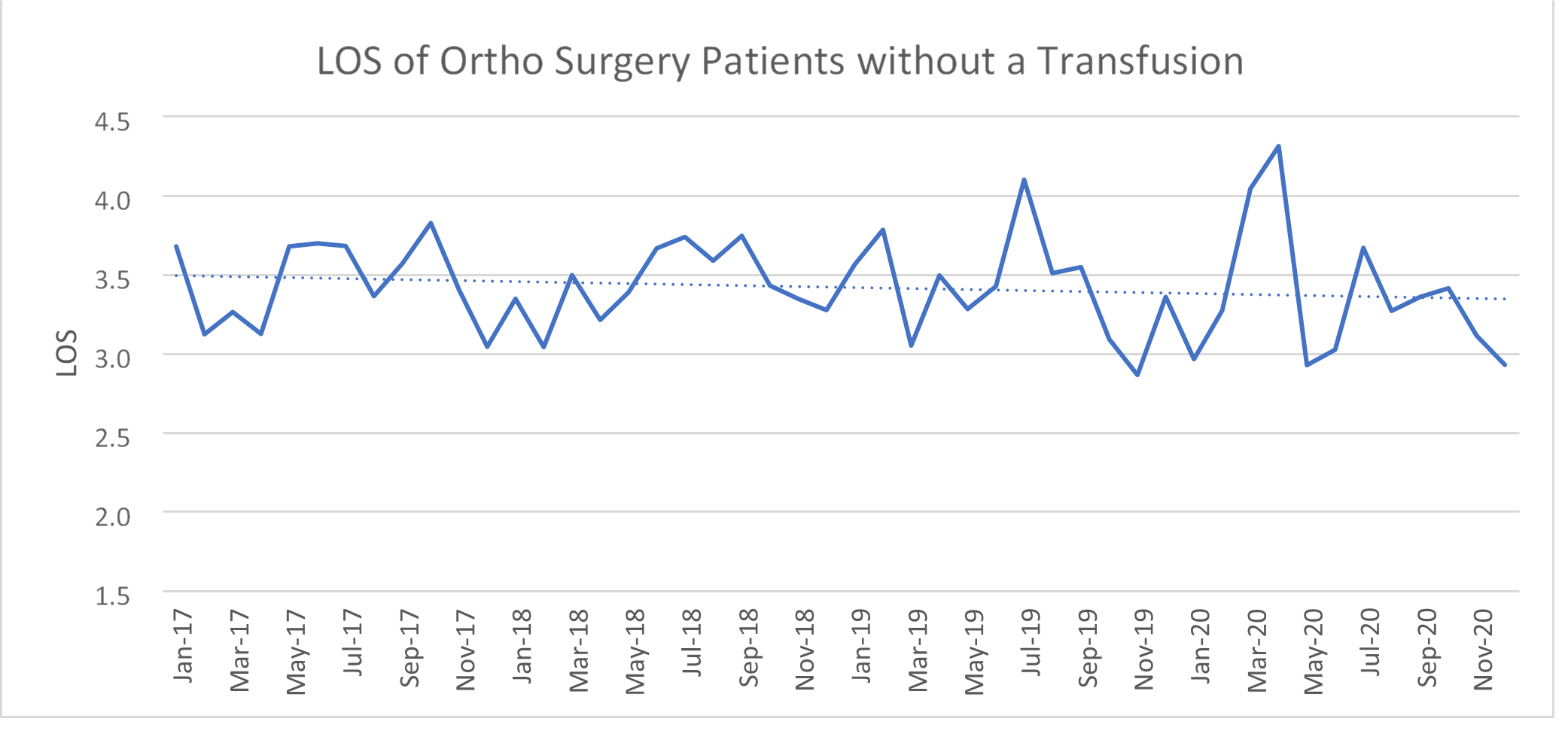
In the ortho surgery patient population — an example of where blood transfusion was decreased, there was no increase in the overall LOS and even with the impact of COVID-19 on hospital operations, there was still a noted decrease in the overall LOS. LOS was also noted to be below the Vizient benchmark.
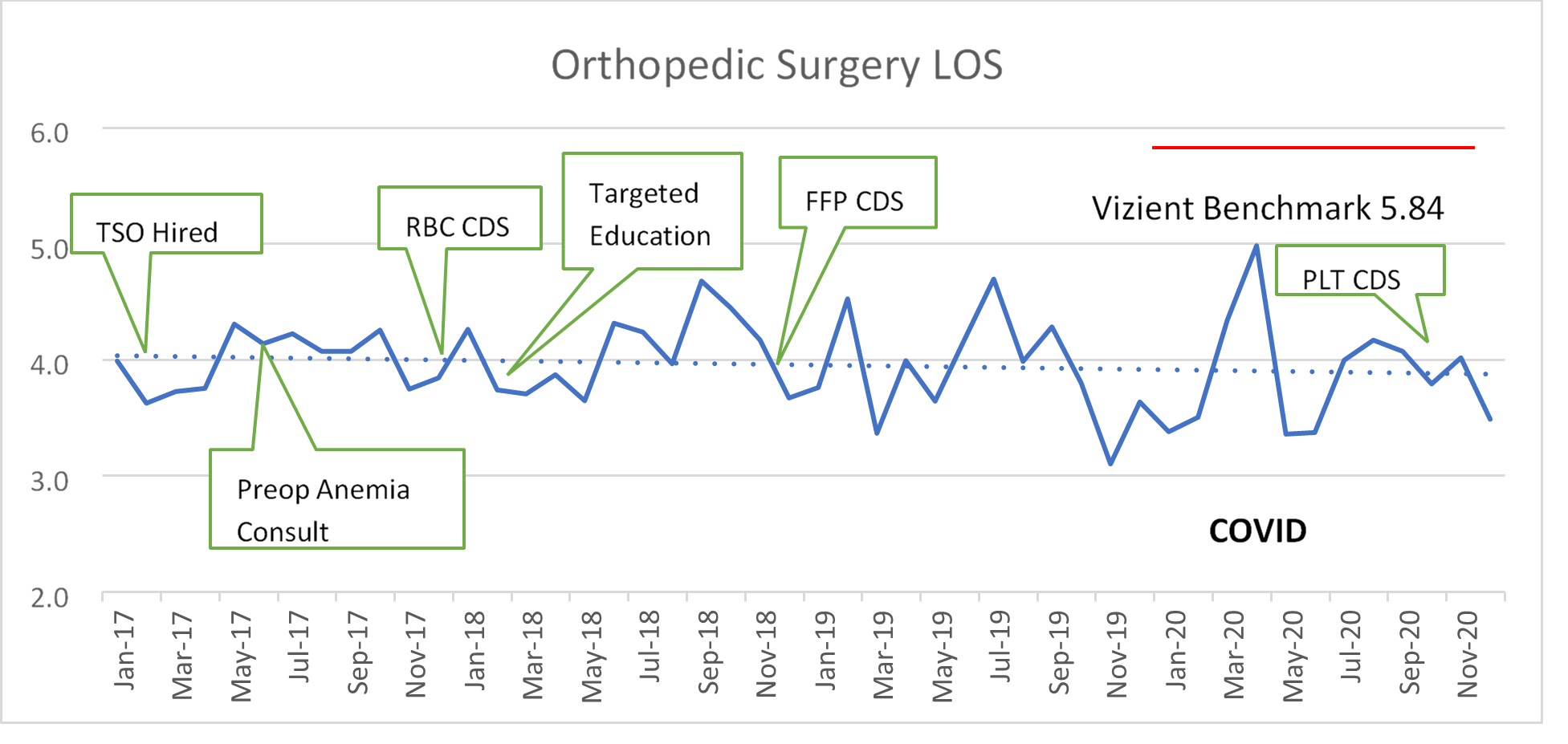
Source: University of Missouri Health Care
In the orthopedic surgery population, there was also a noted decrease in LOS for patients who did not receive a blood transfusion. This supports the standard that transfusing RBCs primarily for a hemoglobin < 7 g/dl did not have a negative impact on the LOS.
Source: University of Missouri Health Care
Nine months after embedding the alert into the electronic health record, staff reduced the health system’s overall RBC transfusion rate by 13.34 percent, saving approximately $195,000 in acquisition costs and avoiding between $505,000 and $1.14 million in indirect costs for things like transfusion administration, patient blood testing and overhead. In the original work, from December 2017 through February 2019, MU Health Care also noted a 10% reduction in the mortality rate of transfused patients.
Accountability and Driving Resilient Care Redesign
MU Health Care utilizes the leadership dyad framework, which is a methodology where the ideal leader is two people. This leadership style encourages open communication and gives room for a collaborative discussion to understand multiple points of view. In healthcare, the leadership dyad model is best described as the pairing of a physician with a non-physician administrator for strategic and operational oversight. In this project, for example, if a provider didn’t adhere to the standard, a pathology leader could have that discussion with the appropriate medical director — there is always a one-on-one communication path and decisions/results are data driven.
The blood management analysis dashboard displays key performance indicator trends and provides information with multiple layers of data with the ability to filter down to individual providers and outcomes. MU Health Care leaders can deliver targeted education on RBC transfusion best practices to departments with high alert override rates when needed. One department’s alert override rate dropped 29 percent a month after receiving targeted education.
Source: University of Missouri Health Care
Access to data that shows the success of the CDS alert for RBCs led MU Health Care to subsequently roll out CDS alerts for FFP, PLTs and an algorithm to identify patients with morbidity issues that may also impact the need to delay surgery or alert for the preop anemia consult.
Examples of data dashboards
Source: University of Missouri Health Care
Source: University of Missouri Health Care
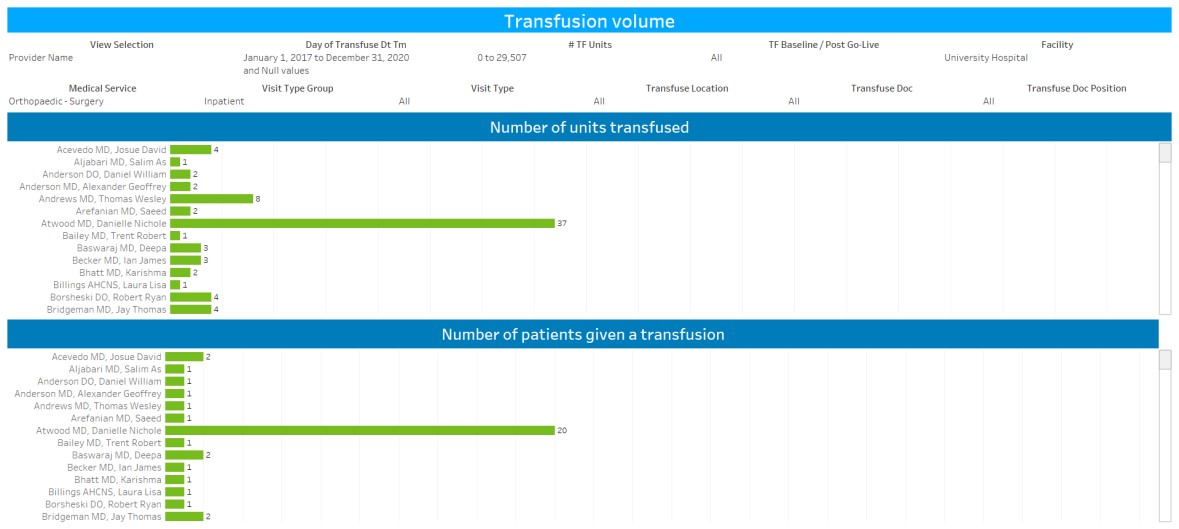
Source: University of Missouri Health Care
Source: University of Missouri Health Care
The views and opinions expressed in this content or by commenters are those of the author and do not necessarily reflect the official policy or position of HIMSS or its affiliates.
HIMSS Davies Awards
The HIMSS Davies Award showcases the thoughtful application of health information and technology to substantially improve clinical care delivery, patient outcomes and population health.



